Rocky Mountain MIRECC TBI Toolkit
Why an Online Toolkit?
This toolkit aims to provide necessary information to address the needs of individuals with a history of TBI and co-occurring mental health conditions. Community mental health clinicians', justice-involved professionals', and Military/Veteran experts' input was integral in identifying areas of focus.
Overview of the Toolkit
TBI 101
Provides background information regarding the physical and mental health impact associated with brain injury. This section also highlights information about populations uniquely at risk for experiencing traumatic brain injuries (Military/Veterans, justice-involved, homeless and youth). Go to TBI 101
Screening and Assessment
Outlines recommended and commonly used screening and assessment tools to help in the identification and evaluation of brain injury and co-
Interventions
Reviews interventions and strategies available to help enhance treatment planning to support brain injury recovery and outcomes. Go to Interventions
TBI Resources
Points healthcare providers, family, caregivers and survivors towards resources that support recovery. Go to TBI Resources
Definitions
- Screening
- Screening refers to a preliminary procedure, such as a test or examination, to detect the most characteristic sign or signs of a disorder that may require further investigation. 5 Screening helps providers identify who might have a history of TBI. A positive screen would suggest the potential need to conduct further assessment to make a determination regarding TBI history.
- Assessment
- Assessment refers to an evaluation or appraisal of a condition based on the patient's subjective report of the symptoms and course of the illness or condition and the examiner's objective findings, including data obtained through laboratory tests, physical examination, medical history, and information reported by family members and other health care team members. 5 Assessment assists the provider in determining whether an individual has a history of TBI. Assessment of co-occurring mental health symptoms and other sequelae is a critical step in providing care to those who have a history of TBI.
- Interventions
- Intervention is defined as an act performed to prevent harm to a patient or to improve the mental, emotional, or physical function of a patient. 5 The interventions referenced in this toolkit are aimed at treating symptoms associated with TBI and common co-occurring mental health conditions.
-
The Purpose
Traumatic Brain Injury (TBI) is a significant public health concern. Survivors of TBI can struggle with both short-term and long-term effects, which may impact several aspects of a person's life, making it difficult to achieve one's goals.
While anyone is at risk for getting a TBI, certain groups face more risk of being affected by TBI than others. Therefore, this toolkit specifically emphasizes TBI in justice-involved, youth, homeless, and Military/Veteran populations.
-
Click/Tap for smaller image
-
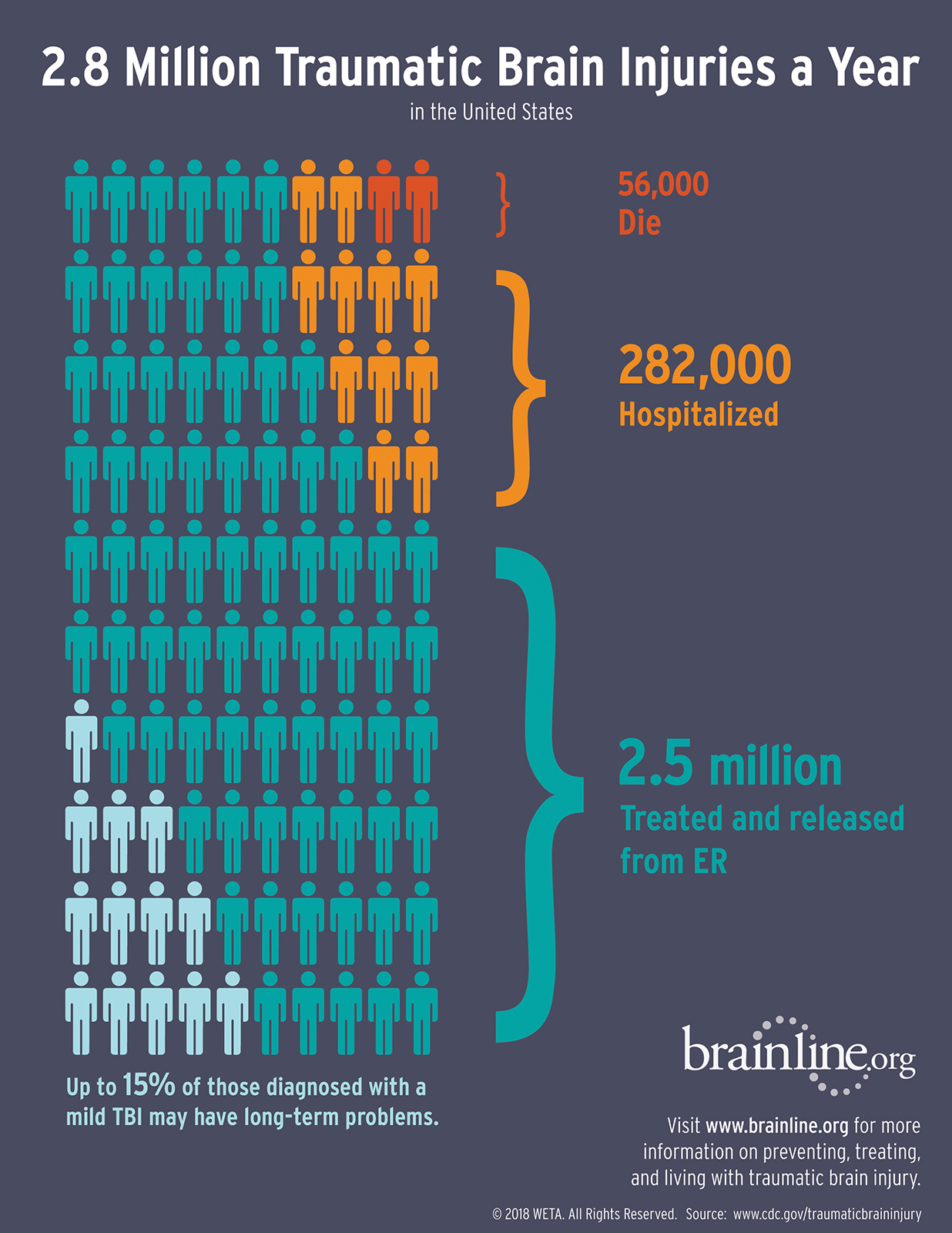
2.8 Million Traumatic Brain Inuries a Year in the United States
56,000 Die
282,000 Hospitalized
2.5 million Treated and released from ER
Up to 15% of those diagnosed with a mild TBI may have long-term problems.
Justice Involved
Among individuals in correctional/detention facilities, the rate of traumatic brain injury has been estimated at 60% in adult offenders and 30% in juvenile offenders compared to the general population (8.5%). In both adult and juvenile justice populations, TBI is associated with poorer outcomes, including reduced engagement in rehabilitation and higher rates of re-offending. 3
51.5% Higher occurrence of TBI in adult offenders than general population
Veterans and Military Personnel
The military conflicts from 2005 to 2018 increased the number of service members and Veterans living with TBI. More than 453,00 U.S. service members were diagnosed with a TBI between 2000 and 2021. 3, 4
> 453,000 Service members with a TBI
Youth
Children (birth to 17 years old) had 16,070 TBI-related hospitalizations in 2019 and 2,774 TBI-related deaths 1 in 2020. TBI represents one of the leading causes of disability and death in children ages 0–4 years and adolescents ages 15–19 years. 1, 3
2,774 TBI-related deaths amongst youth in 2020
Homelessness
People who experience homelessness are 2-4 times more likely to have a history of TBI and are estimated to have a lifetime TBI prevalence of over 53%. This leads to poor physical and mental health outcomes, including an increased risk for suicide. 2, 7
> 53% TBI prevalence amongst homeless populations
As such, professionals in criminal justice settings, community mental health, and VHA require the knowledge and skills to meet the specialized needs of these populations. The Rocky Mountain MIRECC TBI toolkit offers a useful starting point to increase the provision of TBI-related mental health services by community professionals.
 Funding
Funding
This toolkit was developed as part of collaborative projects between the Veterans Integrated Service Network (VISN) 19 Rocky Mountain Mental Illness Research, Education and Clinical Center (Rocky Mountain MIRECC) and MINDSOURCE — Brain Injury Network. The projects were funded by the Health Resources and Services Administration (HRSA) and, more recently, the U.S. Department of Health and Human Services under the Administration for Community Living. The toolkit contains best practices identified at an expert consensus meeting, which were published in the Community Mental Health Journal (Olson-Madden, Brenner, Matarazzo, and Signoracci, 2013). 6 The content is also based on input obtained from Colorado mental health providers and correctional professionals who participated in focus groups aimed at identifying their learning needs regarding working with Veterans and civilians who have a history of TBI and co-occurring disorders.
 Feedback
Feedback
Your feedback is important and helps keep this toolkit relevant and up to date. If you find broken links, out of date information, or you have questions/suggestions, please contact Rocky Mountain MIRECC at RockyMountainMIRECC@va.gov
























