Precision Medicine News
Advancing Discovery: A New Era of Precision Medicine at the Bronx VA
The James J Peters Veterans Administration Medical Center (JJPVAMC) and the VISN 2 Mental Illness Research, Education, and Clinical Center (MIRECC) have recently announced a new Center for Precision Medicine and Translational Therapeutics in collaboration with the Icahn School of Medicine at Mt. Sinai. The mission of the center is to promote precision medicine, defined as “an emerging approach for prevention and treatment that takes into account each person’s variability in genes, environment, and lifestyle.” Precision Medicine is a topic that has been gaining traction in recent years, with many academic medical centers having their own center for precision or personalized medicine. The goal of precision medicine is to better understand the genetic and biological makeup of disease, and using this information, allow for more specified treatment that maximizes efficiency and minimizes side effects.
The center will be led by two experts in the field of precision medicine, Panos Roussos, MD, PhD (Director) and Georgios Voloudakis, MD, PhD (Associate Director). Dr. Roussos is a Professor of Psychiatry and Genetics and Genomic Sciences at the Icahn School of Medicine at Mount Sinai and a JJPVAMC/MIRECC faculty member. He also serves as the Director of the Center for Disease Neurogenomics (CDN) and a member of the Friedman Brain Institute. Dr. Voloudakis is also a member of the Mount Sinai faculty as an Assistant Professor of Psychiatry and Genetics and Genomic Sciences where he leads CDN’s group of Translational Bioinformatics and Precision Therapeutics, and a JJPVAMC/MIRECC faculty member. Roussos and Voloudakis’ work has been frequently published in the top scientific journals, and Roussos is currently the Primary Investigator for six NIH RO1 grants and several VA Merit grants. The center has also employed David Burstein PhD, a mathematician and data scientist. Dr. Burstein’s research in machine learning have led to both improvements in electronic health record data quality , as well as novel scientific discoveries. Dr. Burstein has a new project called “Mitigating Genomic Research Disparities in the Million Veteran Program,” which, according to Dr. Burstein, “will leverage data-driven meta-analyses to identify novel genetic targets for serious mental illness related traits to improve healthcare outcomes for our diverse Veteran population. In particular, our approach allows us to quantify differences in data quality and aggregate multiple related traits from electronic health record data to increase sample size representation across all demographic groups.”
This center is possible thanks to the commitment of JJPVAMC Director, Dr. Balavenkatesh Kanna, who has invested in this center and subsequently given the MIRECC, JJPVAMC and VISN2 access to invaluable expertise and resources. “The Center for Precision Medicine and Translational Therapeutics (CPM2T) is a state-of-the-art research enterprise established at JJPVAMC in collaboration with the Center for Disease Neurogenomics at Mount Sinai Icahn School of Medicine,” Dr. Kanna shared, “We are proud to support cutting edge research by Director Dr. Roussos, and the Precision Medicine team through this center. We are particularly excited about the prospect of this work leading to high-impact advances in care of the Veterans we serve.”
This center is uniquely positioned to conduct innovative research in the field of precision medicine thanks to the breadth of resources provided by the VA. The VA is home to the Million Veteran Program (MVP), the largest genetic database in the world. MVP is a “genetic and health research program” for which over one million Veterans have shared their DNA for research purposes. In addition to this large bank of genetic data, the VA also provides investigators with access to clinical data for over 9 million Veterans, including those in MVP. The primary goal of the Center for Precision Medicine, according to Roussos, is to “use data we have from the Million Veteran Program, but also the overall VA Corporate Data Warehouse to actually promote precision medicine.”
Drs. Roussos and Voloudakis also hope that the work done in the center will promote translational therapeutics: the application of genetic discovery into treatment development. Dr. Roussos shared that there is “a very unique opportunity using data that we have from the VA to really be able to promote new target detection and be able to come up with new treatments, either from medications that we use in other diseases and have never tried in the disease of interest, or come up with new targets and really think about innovative approaches to design new therapeutic or drug delivery approaches that target those specific kind of disease-associated targets.”
Recently, Drs. Roussos, Voloudakis and Burstein have made meaningful discoveries related to Binge-Eating Disorder (BED). Despite being the most prevalent eating disorder according to epidemiological studies (~ 3% of the general and Veteran population), BED is significantly underreported in biobanks (~0.1%). Additionally, because of its common comorbidity with obesity and recent introduction to diagnostic and international disease classification manuals, BED often goes undiagnosed. Using electronic health data from MVP, Roussos and team were able to conduct a machine-learning approach to identify many additional individuals with BED, despite no official diagnosis being noted in their records. With this data, they were then able to conduct a genetic analysis, in which they controlled for body mass index, and were able to identify specific genetic risk factors for developing BED. Additionally, they found shared heritability between BED and other psychological symptoms (e.g., anxiety) and discovered that iron metabolism likely has a causal relationship with BED. These findings were published in Nature Genetics (Burstein et al., 2023). This is an example, per Roussos, of the way that data from MVP, in conjunction with his team’s experience, can facilitate significant discovery in terms of the biological makeup of diseases for which little is known, and subsequently open the door to consider new medications and treatment for these disorders. Additionally, Voloudakis highlighted that it is a priority of the center to make precision medicine more equitable to all veterans regardless of their ancestral genetic background and are committed to conducting genetic analyses using data from marginalized and underrepresented ethnic and racial groups.
In addition to facilitating his team’s own research, Roussos shares that he wants this center to be “an entry for investigators who want to do precision medicine or use the Million Veteran Program Data, but don’t know how.” His goal, he shares, is to bring together a “group of investigators…that have interesting questions and can benefit from the [MVP] data.” Furthermore, Roussos shares his hope that the analysis of MVP data will allow investigators to make “inferences about clinical utility and treatment” that can then be shared with other large academic institutions with the capacity to run large-scale clinical trials. “Our goal,” he stated, “is to support MIRECC in many of the efforts that are happening right now, support many other investigators within the Bronx VA, VISN-2, and nationwide on research that involves diseases that go beyond mental illness. With the currently available resources and expertise, precision medicine and new treatment development and discovery can become reality.” 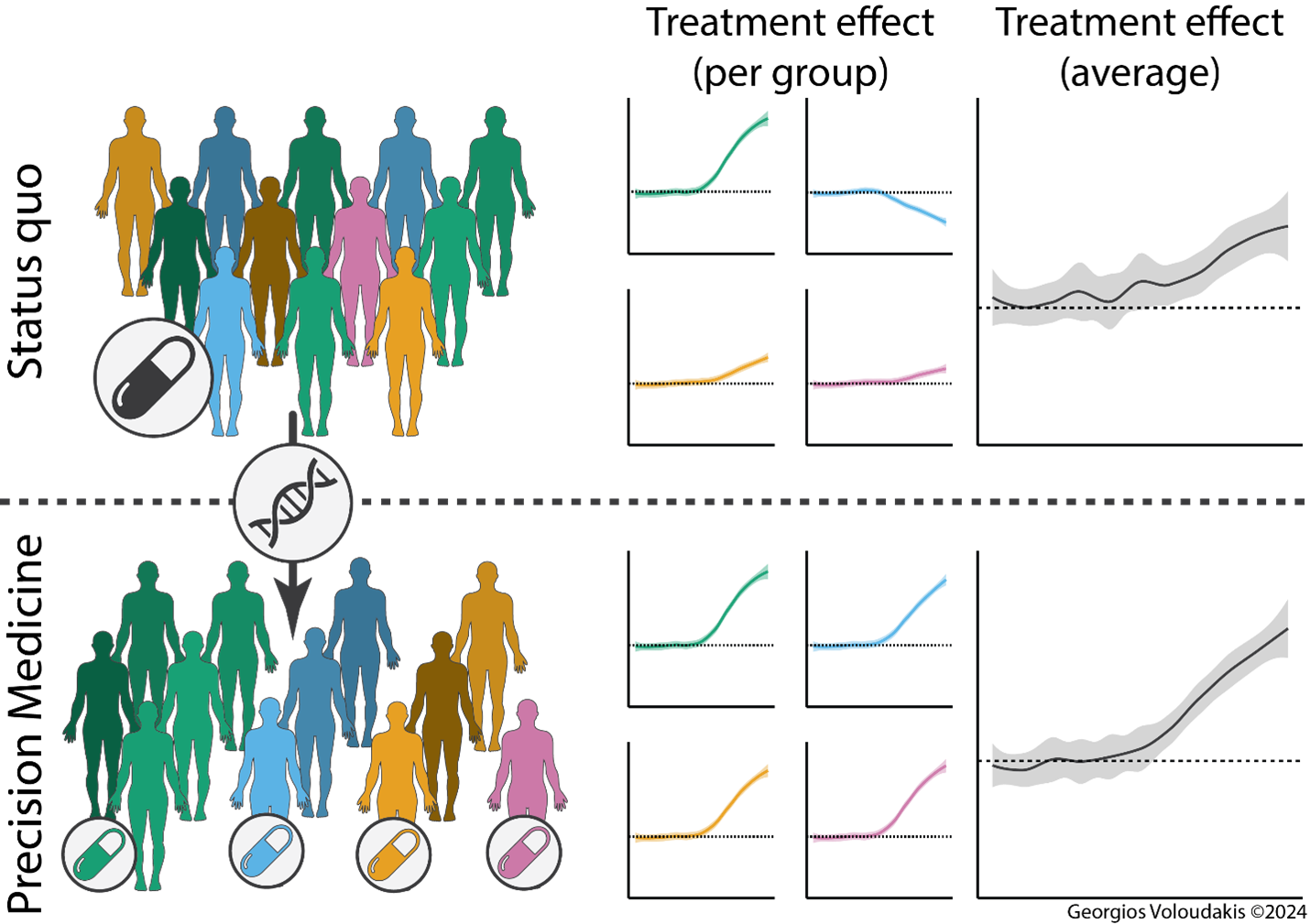
References
Burstein, D., Griffen, T.C., Therrien, K. et al. Genome-wide analysis of a model-derived binge eating disorder phenotype identifies risk loci and implicates iron metabolism. Nat Genet 55, 1462–1470 (2023). https://doi.org/10.1038/s41588-023-01464-1



















