Sierra Pacific (VISN 21) MIRECC

Education Overview
Education and Dissemination provides the most current information related to dementia and PTSD and evidenced-based practices. The goals are:
- to disseminate the latest evidence-based practices and peer-reviewed research to Veterans, family members and clinicians,
- to address the education needs of VA clinicians in VISN 21, and
- to support the VA Office of Mental Health in the national implementation of evidence-based practices.
Dementia
PTSD
TMS
Psychotherapy
Dementia
Dementia Education Overview
Contacts
Director: Allyson Rosen, Ph.D., ABPP-CN
Continuing Education on Alzheimer’s Medications and Tests
Approval for: ACCME, ACCME-NP, ANCC, AOTA, APA, ASWB, JAIPCE, NYSED, NYSED-P
A Disease-Modifying Therapy for Alzheimer’s Disease (AD). What is it?
It is important for older people with memory and thinking problems to seek a comprehensive evaluation from a healthcare professional because these problems can have many different causes. For some people, these problems may be related to Alzheimer’s disease brain pathology, including high levels of a protein called amyloid. A drug was recently approved that reduces amyloid levels and slows cognitive and functional decline. The treatment must be given via IV infusion every two weeks. Although most patients tolerate the treatment without difficulty, some patients have brain swelling or brain bleeding; to monitor for this, patients must undergo brain scans periodically.
WEBINAR
Speakers: Peter Ljubenkov, UCSF, Steven Chao, Palo Alto VA/Stanford
See Also Managing ARIA (Alzheimer’s Association)
How is Brain Pathology Detected and How is Measuring it Used in Dementia Diagnosis?
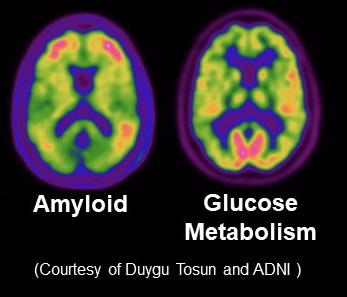
Clinicians use biomarkers, tests that reflect certain biological processes. Biomarkers for brain amyloid are used to assist in the diagnosis of Alzheimer’s disease and identify individuals who may be candidates for amyloid-lowering treatments. Biomarkers for Alzheimer’s disease including neuroimaging such as PET scans and concentrations of key proteins in the cerebrospinal fluid or blood.
WEBINAR
Speakers: Suzanne Schindler, Washington University, Allyson Rosen Palo Alto VA/Stanford
Are these Drugs and Tests FDA Approved and What Does that Mean?
There are different types of approval for drugs and biomarker tests. Alzheimer’s disease treatments and diagnostics are rapidly advancing and it is vital to understand what different types of approval mean to make informed choices.
WEBINAR
Speakers: Nadezda Radoja, NIA, Michelle Mielke, Wake Forest University
Issues Surrounding Communicating Biomarker and Genetic Information
Biomarkers and genetic tests are increasingly important in the clinical evaluation and treatment of Alzheimer’s disease. For example, Alzheimer’s disease-specific treatments require biomarker testing for confirmation of amyloid pathology and recommend APOE genotyping for assessment of risk for treatment complications. This webinar discusses best practices in disclosure of test results as well as ethical concerns related to these tests.
WEBINAR
Speakers: Scott Roberts, U. Michigan, Emily Largent, U. Pennsylvania
Further Reading: Learn more
Related Ongoing Research
Alzheimer's Neuroimaging Initiative (ADNI)
The Alzheimer’s Disease Neuroimaging Initiative (ADNI) is a longitudinal multicenter study designed to facilitate drug development by validating clinical, imaging, genetic, and biochemical biomarkers for the early detection and monitoring of Alzheimer’s disease (AD).
Ongoing Community Outreach
Advisory Group on Risk Evidence Education for Dementia (AGREEDementia.org)
ADNI revealed some brain changes leading to dementia begin decade before symptoms and there are now brain scans and blood tests as well as treatments clinically available in part due to ADNI. AGREEDementia is a collaboration with Stanford’s Alzheimer’s Disease Research Center and is national partnership between scientists, clinicians and the community to help people learn about this dementia risk information and help guide how it is used and shared. We meet monthly and there are lectures.
Contact: Allyson Rosen
Protecting Progress: Ethics Review Description and Publications
As innovations in dementia develop, there are often concerns about how they are best applied. Ethics review focuses on solutions to barriers to implementation through work with the Journal of Alzheimer’s Disease.
Learn more
Contact: Allyson Rosen
Annual Updates on Dementia
For more than 20 years, we have provided continuing education on the latest developments in dementia diagnosis and care in partnership with the Alzheimer’s Association, GRECC, Family Caregiver Alliance, the Ombudsman of Santa Clara, and the Stanford Alzheimer’s Disease Center among others.
Contact: Allyson Rosen
Geriatric Education Rounds:
An ongoing lecture series with faculty and internationally recognized presenters and collaboration with Stanford’s Department of Psychiatry and Behavioral Sciences.
Contact: Sherry Beaudreau
Hospital Dementia Committee
The Dementia Committee is an inter-professional committee which increases awareness of issues related to dementias, and promotes collaborative efforts regarding clinical activities, education, and research activities in this area. The committee reports to the Medical Executive Committee (MEC) and the VISN Dementia Committee.
Palo Alto VA contact: Allyson Rosen, Dat Hoang-Gia (GRECC Partner)
Request a Presentation
Products
Geriatric Depression Scale (GDS)
Receiver Operator Characteristics (ROCS)
Memtrax Online Research Cognitive Screening (now part of ADNI)
Collaborating Organizations
Stanford Alzheimer’s Disease Research Center (ADRC)
Stanford VA Alzheimer’s Center
Geriatric Research Education and Clinical Center (GRECC) Palo Alto
GRECC Geri Scholars
Other Aging-Related
Epidemiology: Aging Women Veterans
The Women’s Health Initiative represents a large, longitudinally studied, group of women Veterans and civilians who participated in a study of hormone replacement. The group is special because they have been very carefully described in terms of their health and cognition. The attached link has multiple papers describing how older women Veterans have different outcomes from civilians as they both age.
Contact, Julie Weitlauf.
Learn more
Implementation: Improving Brain Stimulation with Imaging (IBSI)
Repetitive pulse TMS (rTMS) is a major focus of our center and an important therapy that enhances brain functioning. Our center applies it to dementia and mild cognitive impairment. Unfortunately, most clinical rTMS clinics do have access to MRI’s and hence use scalp landmarks to direct rTMS therapy to a selective brain region. This program applies multi-site fMRI to study variations in brain targeting which relates this information to clinical outcome. Contact: Allyson Rosen
PTSD
PTSD Education Overview
Contacts
Director: Leanne Williams, PhD
Other Educators:Joseph Ruzek, PhD, Julie Weitlauf, PhD
What is PTSD?
Posttraumatic stress disorder (PTSD) can occur after someone goes through a traumatic event like combat, assault, or disaster. Most people have some stress reactions after a trauma. If the reactions don't go away over time or disrupt your life, you may have PTSD.
Additional patient information
Dissemination of Best Practices
We provide webinars and talks as needed on topics of relevance to our community of clinical professionals and Veterans. We hold an annual “Updates on PTSD” webinar conference. This webinar also incorporates emerging topics of relevant to clinical professionals and Veterans, including precision medicine and implementing approaches for improving outcomes for PTSD and comorbid disorders. To ensure cutting-edge information is disseminated widely beyond the day of the webinar itself we host a video of the webinar online whenever possible. We partner with educators at Stanford University and the University of California San Francisco in order to provide the highest quality education and insights.
Supplementing these webinars are more specialized presentations on topics initiated by VA health professionals and educators or by our community. For example, throughout 2020 through to the present we have hosted a case series focused on novel therapeutics such as transcranial magnetic stimulation for PTSD and related disorders such as major depressive disorders.
Major Resource
Our major resource for integrated information for the public and for professionals is the National Center for PTSD. http://www.ptsd.va.gov
Ongoing Community Outreach
Major Initiatives Supporting Research Cores
In support of the clinical dissemination of research, we are developing a new program focused on precision medicine approaches for PTSD and comorbid disorders in Veterans. Under this new program, we address the goals of the “Precision Medicine for Veterans Initiative”, as outlined in the Commander John Scott Hannon Veterans Mental Health Care Improvement Act of 2019. We are using functional brain imaging, electroencephalogram, and behavioral clinical measures to develop innovative diagnostics that identify which Veterans will benefit most from different therapeutic options. We also develop the clinical translational understanding of innovative interventions spanning TMS, ketamine, and exploratory therapeutics. This initiative is anchored in the understanding of brain circuits and cognitive functions and the daily functions they implicate. The goal is to tailor recovery in a more precise way based on the capacity and needs of each Veteran, to optimize daily social and vocational function, and minimize disability and risk for suicide.
TMS
TMS Education Overview
Click the map for specific clinic contact information.
Contacts
Please contact the Director of the National Clinical rTMS Program, Michelle Madore, PhD, Clinical Neuropsychologist: Michelle.Madore@va.gov or Program Specialist L. Chauncey Green: Laroman.Green@va.gov
Others Providing TMS Education: Mark George, MD, Allyson Rosen, Ph.D., ABPP-CN
What is transcranial magnetic stimulation (TMS)?
TMS is a clinical tool used to change activity in the brain without drugs. TMS therapy works by placing a special coil on the head that delivers magnetic pulses which, over several sessions, cause those stimulated regions to function better. A great description of TMS may be found on the NIMH website here.
Dissemination
The National Pilot Program is a Mental Health Funded pilot project which began in FY 2017 to expand access to TMS. The effort is based upon the work of Dr. Yesavage as PI of Co-operative Study (CSP 556) in treatment resistant major depression disorder (TRMDD) in Veterans. rTMS is FDA approved for treatment resistant major depressive disorder. This effort focuses on starting TMS clinics in the VA and includes purchase of rTMS equipment, assisting in staff training, aiding in developing VA documentation including credentialing and hospital center memoranda, clinical consultation, and evaluation of national Veteran response to TMS Therapy.
Program Goals
- Open and Support TMS Clinics in the VA
- Coordinate Purchasing TMS Machines through a National Bidding Process
- Educate TMS Prescribers and Operators
- Evaluate Veteran response to TMS through Outcome Data Collection as part of Program Evaluation
- Provide Ongoing Continuing Education
- Assist with Credentialing and Administrative Set-up
- Develop Model Memoranda and Procedures
Products and Education
Psychotherapy
Psychotherapy Education Overview
Contacts
Edward Wakabayashi
Dissemination
About the Dissemination. MHS has continued to disseminate Acceptance & Commitment Therapy (ACT) for Depression, Cognitive Behavioral Therapy for Depression, (CBT-D), and Cognitive Behavioral Therapy for Insomnia (CBT-I) in VHA. VISN 21 MIRECC works as local coordinator with MHS to implement these programs offered to VA clinicians nationwide. Over 2000 VA clinicians have attended in-person trainings for these initiatives.
Return to Home page



















