Newsletters | South Central MIRECC
Spring 2018, Volume 20, Issue 3 - In this Issue
Research to Practice: Implementation of PC-MHI in Challenged Settings - A Qualitative StudyFall 2017 SC MIRECC Motivational Interviewing Training
Dr. Lilian Dindo Selected as New Houston Anchor Site Leader
Clinical Demonstration Project - FLOW
Pilot Study Research Program Applications Due July 2
Implementation, Design and Analysis Support Available for Affiliates
Clinical Demonstration Project - FLOW
By Dr. Tracey L. Smith, SC MIRECC Associate Director for Improving Clinical Care
FLOW is a clinical demonstration project developed and supported by the SC MIRECC (led by Dr. Tracey Smith, Associate Director for Improving Clinical Care) in coordination with VISNs 16 & 17 mental health leadership. The goal of FLOW is to improve access to VA mental health services by facilitating the transition of Veterans enrolled in mental health clinics who are recovered/stable back to primary care. The project was developed to optimize access to mental health (MH) clinics at VA medical centers. Delayed access to MH services affects Primary Care (PC) and Primary Care-Mental Health Integration (PC-MHI), that must provide mental health care to Veterans who are waiting for appointments in MH clinics.
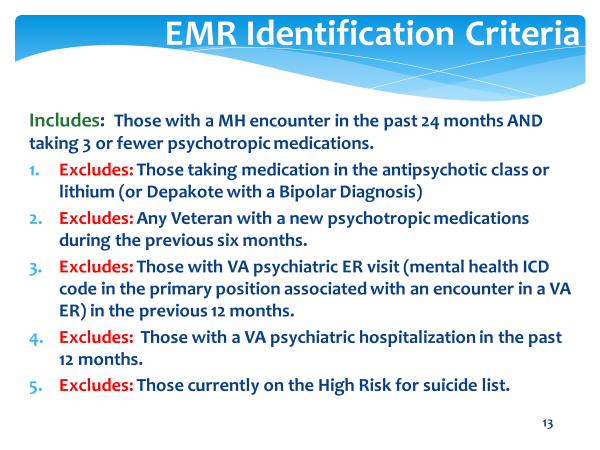
The FLOW project developed criteria to identify Veterans in the electronic medical record (EMR) that appeared to be recovered/stabilized. These criteria were used to create the online MH FLOW report that can be accessed by VA providers and administrators (with appropriate access credentials). Data from the MH FLOW report can be exported and sorted by upcoming appointment date and provider name. Providers can then review their patients on the list and decide whether to discuss the transition with the Veteran. Names of the Veterans eligible to transition to PC are sent to their MH provider for review. If the provider agrees, the recommended return to PC is discussed with the Veteran. If the Veteran concurs, the Veteran is transitioned to PC. MH providers use a templated progress note (for tracking a Veterans return to PC) co-signed by the Veteran’s PC provider.
FLOW has been fully implemented at one VISN 17 site (McAllen, TX) and is beginning at three other sites (Houston, TX, Temple TX, and Jackson, MS). Data from McAllen, TX demonstrated that of the 2,634 Veterans who were identified as being recovered/stabilized in a nine-month period, 341 had their care transitioned to PC (13% of those identified in the report). During that same time period, only nine (2.6%) returned to MH and two of those had brief psychosocial crises and then returned to PC. These very early results suggest that it is feasible and effective to use EMR criteria for identifying recovered/stable MH Veterans who may be candidates for transition to PC, thus increasing access to MH services for Veterans with acute or chronic needs.
Based on early data, the Office of Mental Health and Suicide Prevention (OMHSP) has asked the SC MIRECC FLOW team to implement this project nationally. We are working with Dr. Jodie Trafton and her team at the Program Evaluation and Research Center in Palo Alto so they can adapt the MH FLOW report for all VA’s. We are also working with OMHSP on a national implementation and technical assistance plan.
Last updated: December 15, 2020



















