MIRECC / CoE
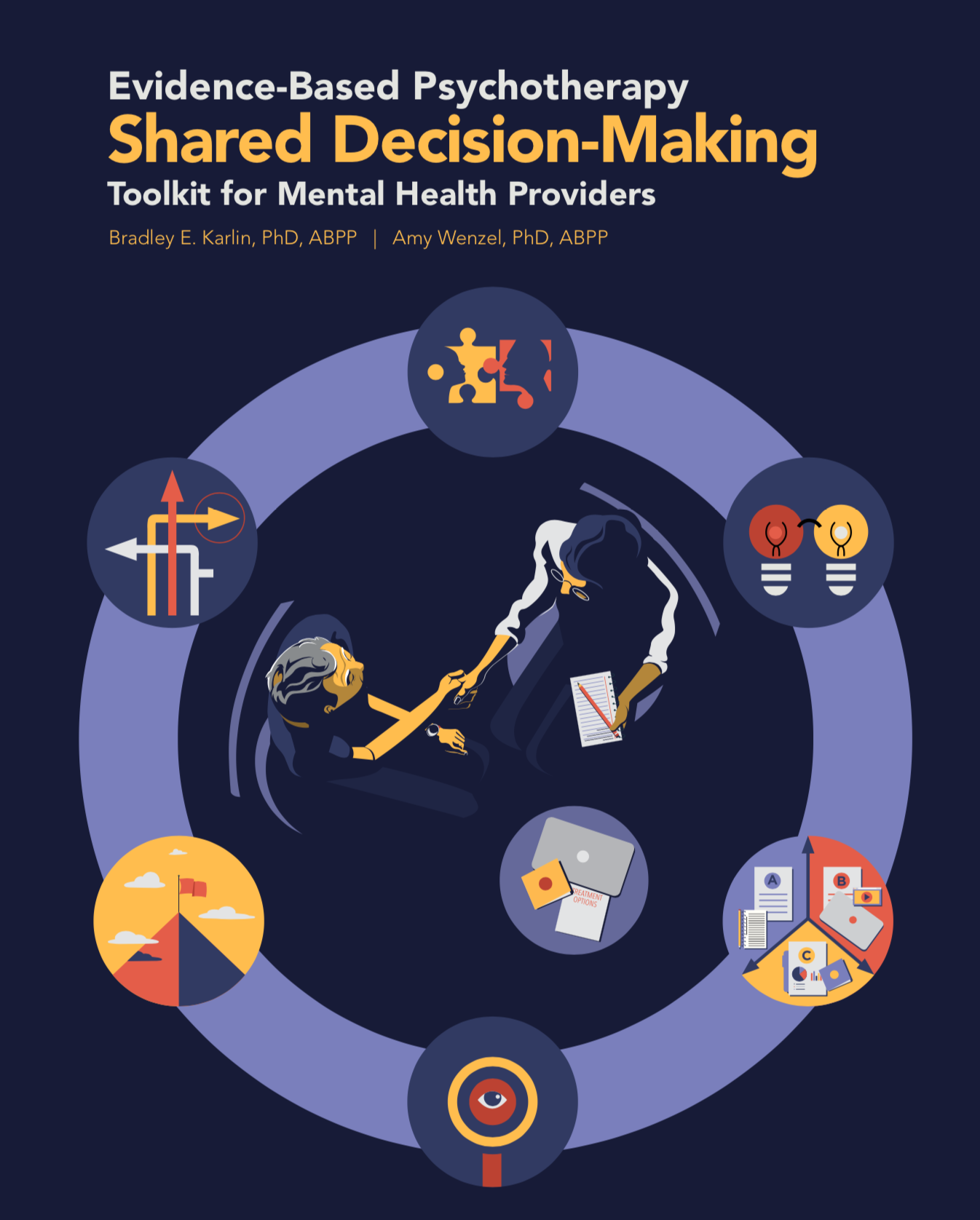
Evidence-Based Psychotherapy Shared Decision-Making Toolkit for Mental Health Providers
Introduction to Toolkit
This toolkit contains information and resources to promote Veterans' engagement in evidence-based psychotherapies (EBPs) through the use of shared decision-making, beginning prior to the initiation of treatment. Increasingly part of high quality, patient-centered care in other health care contexts, shared decision-making principles and processes provide significant opportunities for promoting initial and ongoing engagement in EBPs.
The primary focus of this toolkit is on identifying key components and steps for implementing a pre-treatment Shared Decision-Making (SDM) session to increase initial engagement in EBPs. This SDM Session is a highly collaborative process designed to promote informed choice, treatment motivation, and patient readiness for EBP. The SDM Session includes 6 key components.
Connect
Motivate
Educate
Explore
Set Goals
Choose
In addition to providing tools to promote initial engagement, the toolkit includes treatment process and related resources for increasing ongoing engagement for Veterans who choose to receive EBPs. This toolkit is made available as a public education resource to support mental health providers and program administrators both within the VA health care system and in the community.
Although the focus of this toolkit is on promoting the engagement of Veterans in evidence-based psychotherapies, the principles and processes of shared decision-making, informed choice, and patient engagement described in the toolkit offer opportunities for enhancing the treatment experience and maximizing outcomes more broadly. Indeed, the concepts and strategies recommended in the toolkit represent core components and processes for maximizing engagement and outcomes that may also be incorporated into other types of mental health services.
On this page:
Shared Decision-Making and EBP 
Open toolkit PDF to this section (Page 17)Many Veterans initially present for care unfamiliar with mental health treatments, how they may be beneficial to their personal situations, and what they would like to see change in their lives. Veterans also often have differing perceptions of treatment, past treatment experiences, and reasons for seeking care. These patient factors serve as significant gaps to seeking and engaging in EBPs. Addressing these factors and promoting provider-patient alignment and partnership is critical prior to treatment selection and initiation.
The Shared Decision-Making (SDM) session is a highly collaborative process designed to empower Veterans with information for making an informed choice about treatment and for increasing treatment motivation and readiness prior to the initiation of EBP or other mental health treatment.
The SDM Session is rooted in the premise that when patients or clients are informed about treatments, provided with an opportunity to examine concretely how treatment may be valuable to their lives, and directly involved in the decision about the treatment they will receive, they will be more likely to pursue treatment and be actively engaged in the treatment process. The SDM Session includes both informational and treatment process components designed to increase treatment knowledge; instill accurate treatment expectations; enhance hope, motivation, and trust; promote readiness for treatment; and actively engage Veterans in treatment selection.
The SDM Session (Page 20)
The SDM Session includes the 6 key steps for promoting Veteran engagement and informed choice prior to the initiation of treatment.
Developing a strong interpersonal connection with the Veteran—beginning at the very first encounter—is the foundation of shared decision-making and is essential to promoting treatment motivation and engagement. This is especially significant in the context of individuals with mental health conditions for whom disengagement, avoidance, detachment may be common. An intentional focus on establishing interpersonal connection is often especially important for ensuring trust, which is a necessary ingredient for treatment engagement. The process of promoting interpersonal connection is interwoven throughout the session and is achieved through demonstration of empathic understanding, warmth, genuineness, and collaboration. This section of the toolkit provides specific information and guidelines for establishing interpersonal connection and trust during the SDM Session.
Motivation for change and treatment are essential to initial treatment engagement, ongoing attendance and participation in the treatment process, and degree of treatment response. This step of the SDM Session involves assessing and enhancing the Veteran's motivation for treatment using non-directive questioning to examine reasons for seeking treatment, past treatment experiences, and the benefits and consequences of symptoms.
When patients themselves come to informed decisions to receive a particular treatment, they are more likely to follow through with and actively engage in treatment. This key component of the SDM Session, therefore, involves empowering Veterans with information about available and recommended treatment options so that can make an informed choice about treatment. This includes providing education about EBPs (and other treatments, as appropriate), effectiveness of treatment, and the treatment process. Provider and patient education tools for specific treatments are included in this section to facilitate and help standardize this treatment education process. In addition to promoting informed choice, the process of education allows for identifying and discussing patient questions or concerns and for instilling accurate and positive treatment expectations.
In addition to educating patients about treatment options to promote informed choice, treatment options should be considered in the context of the patient's values and preferences. This section of the toolkit provides specific questions and clinical dialogue to assist providers in exploring Veterans' values and preferences to help inform decisions about specific treatments and promote treatment engagement.
Helping patients to elucidate how therapy may be helpful to them can be a powerful motivator for treatment. Identifying personally relevant ways in which treatment could improve one's life can bring concepts of treatment and treatment effectiveness from a general, abstract level to a more meaningful, individual level and make treatment more real and accessible. Moreover, Veterans presenting for care often have unclear life goals, making treatment goals even less identifiable initially. Furthermore, identifying possible treatment goals can help the provider in offering and providing specific information about treatment options best suited to the patient. This step of the SDM Session involves engaging Veterans in a collaborative process of goal setting to identify potential goals for treatment—to be refined and completed during the beginning phase of treatment — for increasing awareness and motivation and guiding treatment selection. This section of the toolkit provides guidelines, clinical dialogue, and forms for aiding providers in implementing collaborative goal-setting as part of the SDM Session. The Veteran EBP Public Awareness and Engagement web platform—the companion Veteran EBP web portal to this provider portal—also includes interactive goal setting exercises that providers may use with and recommend to Veterans as part of the SDM process.
The final step of the SDM Session is the selection of treatment or other next steps. Empowered with information about treatments and choice, considered through the lens of personal values, preferences, and goals, the patient and provider arrive at a decision for positive change.
Some Veterans, particularly those in severe distress with limited baseline coping skills, may benefit from preparatory work to shore up basic skills and establish greater psychological readiness for treatment. For these Veterans, the toolkit provides an optional preparatory skills building protocol for promoting psychological readiness for treatment. Provider Tip Sheets, incorporating scripts for teaching preparatory skills, and Patient Handouts are provided to facilitate the implementation of this brief pre-treatment intervention.
Checklist for Conducting SDM Session (Page 207)
A summary SDM Session Provider Checklist for guiding the SDM process in session
Putting SDM into Practice: Practical and Logistical Guidelines and Considerations (Page 68)
This section provides guidelines and considerations for locally implementing the SDM process. While the steps of the SDM Session (the "what") are, in general, fairly standard across specific EBPs and conditions, the specific process for executing these steps (the "how") will vary across settings. For example, the length and specific format (e.g., individual vs. group, location, clinician therapist or facilitator) of the SDM Session will vary depending on clinical setting, Veteran patient population served, available resources, and other factors.
Promoting Ongoing Engagement 
Open toolkit PDF to this section (page 79)Therapeutic Alliance (Page 80)
A key clinical strategy for promoting ongoing engagement and retention in treatment is the establishment and maintenance of a strong therapeutic alliance. Although sometimes mischaracterized as less important in the delivery of EBPs relative to other therapies, EBPs delivered well require important and ongoing attention to the therapist-patient relationship and related process requirements. This section describes specific strategies and tools for assessing and enhancing the therapeutic alliance in the delivery of EBPs with Veterans.
Measurement-Based Care (Page 101)
Incorporating ongoing assessment of clinical outcomes in the delivery of EBPs with Veterans is important for monitoring treatment response, providing decision support, ensuring therapist-patient alignment, and promoting ongoing engagement in treatment. This section provides guidance and strategies for integrating assessment of outcomes into the delivery of EBPs with Veterans.
Patient Education Video on Bringing Shared Decision-Making to Mental Health Care
Decision Aids 
Patient decision aids and related resources for use during the Educate step of the SDM Session are available on on the Decision Aids and Treatment Fact Sheets page. A customizable table of treatment options for depression, insomnia, and substance use allows you to remove unwanted treatment columns and add your own if you choose.
Clinician EBP Resources 
This section brings together a variety of clinical and information resources to support mental health and non-mental health clinicians who work with Veterans within the VA health care system and the community.
Questions or problems? Contact Rocky Mountain MIRECC.
Site Map
Contact Information
Colorado
Rocky Mountain Regional VAMC (RMR VAMC)
1700 N Wheeling St, BLDG A2
Aurora, CO 80045
303-399-8020
RockyMountainMIRECC@va.gov
Utah
VA Salt Lake City Health Care System
500 Foothill DR
Salt Lake City, UT 84148
801-582-1565 ext 2835