MIRECC / CoE
Translational Model | Rocky Mountain MIRECC for Suicide Prevention
 |
|||
 |
 |
 |
 |
What is the translational model?
The translational model is a framework for scientific research. It is also sometimes called the translational science spectrum (National Institutes of Health). In the translational model, research happens across five phases, each phase building upon and informing other phases. Many fields use the translational model, including our approach to suicide prevention research.
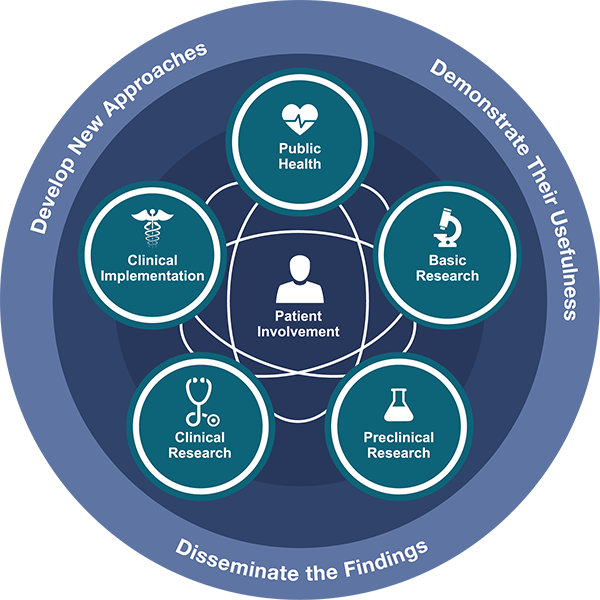
This image from the NIH National Center for Advancing Translational Sciences outlines each phase of the Translational Science Spectrum, also known as the Translational Model.
How do we apply the Translational Model to Veteran suicide prevention research?
At the Rocky Mountain MIRECC we study many different parts of suicide prevention, often at the same time. In the early phases of the translational model (basic research and preclinical research), we look at risk and protective factors for suicide at the most basic level. For example, what role does brain chemistry play in anxiety or depression?
Building on information gained from early phases, our researchers start to formulate theories and begin testing possible approaches to suicide prevention. We test how these methods work in controlled settings (clinical research), in routine practice settings and across different patient populations and communities (clinical implementation and public health). Findings from each phase help identify next steps for suicide prevention research. Across each of the five phases, we emphasize patient involvement and collaboration to ensure our research also incorporates Veteran and community voices.
What are the advantages to using the Translational Model?
The translational model advances our understanding of suicide and suicide prevention in a thorough, progressive way that provides solid evidence for treatments VA and community care provides.
- Find and address gaps: What’s missing? This model highlights what we don’t know and what we need to find out to improve treatments and suicide prevention strategies.
- Identify targets for change: The more we know about contributing risk factors and protective factors, the more likely we are to pinpoint where and how we can make a positive difference.
- Apply knowledge to the real world: Knowledge can get “stuck” unless it moves forward from the lab to the places where Veterans receive treatment and support. The final phases ensure our work reaches Veterans.
Phases of the Translational Model in Suicide Prevention
Select each button to learn more about each phase in the translational model.
The below descriptions are adapted from the NIH National Center for Advancing Translational Sciences.

Basic research explores the biological basis of a disease or behavior. For instance, basic suicide prevention research may explore how certain brain chemistry or genetic factors may directly or indirectly be linked to conditions underlying suicide risk and protective factors.
Preclinical research applies basic science concepts to human medicine. In suicide prevention, preclinical research is used to identify potential new treatment targets or testing a new model or theory.

Clinical research tests the safety and effectiveness of interventions in humans. An example of suicide prevention clinical research could be testing a new individual or group therapy. This research phase includes clinical trials.

Clinical implementation involves putting effective interventions into clinical practice. In suicide prevention, an example would be gathering feedback from the clinicians or patients who tried a new intervention to identify what worked and what may need to be improved.

Public health research looks at population-level health outcomes and the implementation of effective care in communities. Suicide prevention focused public health research may examine trends across communities to identify promising cultural, societal and clinical interventions and care settings.
To see examples of our research studies across the spectrum of the translational model, check out Our Research.
Quick Links to Study Websites
- Understanding Transgender and Gender Diverse Veterans’ Experiences, Needs, and Preferences
- VA Patient Safety Center of Inquiry - Suicide Prevention Collaborative (PSCI-SPC)
- Home-Based Measurement of Circadian Timing in Veterans with Traumatic Brain Injury and Insomnia (Home Circadian)
- Promoting mental health wellness and safety among Veteran firearm owners (FFAST)
- Assessing Social & Community Environments with National Data (ASCEND)
- Suicide Risk and Prevention among Asian American and Pacific Islander Veterans
- Military and Veteran Microbiome: Consortium for Research and Education (MvM CoRE)
- Facilitating Assessment of At-Risk Sailors using Technology (FAAST)
- Advancing Suicide Prevention for Underserved Veterans (ASPIRE) Lab
Site Map
Last Updated 26 August 2024



















