MIRECC Presents Archive 2023-2024
MIRECC Presents Archive
June 5, 2024: Attentional Risk Factors for PTSD: Theory, Research, and Practice
Kate Clauss, PhD
Purpose Statement: Attentional factors are commonly impaired among individuals with posttraumatic stress disorder (PTSD), though they are infrequently addressed in treatment. This lecture will delve into the role of attentional risk factors in the development and maintenance of PTSD. Strategies will be presented for intervening to optimize attentional functioning, which may improve treatment engagement and PTSD symptoms. Participating in this lecture will equip clinicians with evidence-based strategies designed to improve quality of life and functioning among those with PTSD.
Learning Objectives
- Describe how attentional factors contribute to PTSD
- Consider how attentional functioning might influence Veteran’s experience of PTSD and treatment engagement
- Discuss the state of the literature regarding existing interventions for attentional functioning
May 15, 2024: Optimizing sleep for Veterans with chronic pain: Pain, Activation, & Sleep Skills (PASS)
Aaron Martin, PhD
Purpose Statement: Chronic pain is a common among those seeking care in VA, and is highly comorbid with mental health conditions. While different behavioral strategies are available to treat pain-related conditions, sleep is often an under-addressed area. The goal of this lecture is to equip mental health professionals with the knowledge and skills to optimize sleep in veterans with chronic pain. The session will delve into a deep understanding of the relationship between pain and sleep, and discuss evidence-based strategies for improving sleep disturbance in the context of chronic pain
Learning Objectives
- Understand the relationship between pain and sleep, recognizing biopsychosocial mediators
- Identify benefits and challenges to addressing insomnia/sleep disturbances in the context of chronic pain
- Consider treatment modifications and messaging for triage and care to address sleep disturbances in the context of chronic pain
April 17, 2024: Population-based Screening for Suicide Risk: Promises and Limitations
Steve Dobscha, MD
Purpose Statement: Reducing death by suicide is among the highest priorities for VA mental health care. How and when clinicians assess suicide risk can have an impact on patient willingness to engage in treatment. This seminar will review evidence-based strategies for screening for suicide risk and provide recommendations for clinical practice.
Learning Objectives
- Review key elements of the evidence base supporting population-based screening for suicide risk.
- Describe overall benefits and limitations of suicide risk screening
- Identify “best practices” for screening for suicide risk and apply to one’s practice
April 3, 2024: Predictors of PTSD treatment utilization and optimizing treatment for those at risk of poor outcome
Rebecca Sripada, PhD
Purpose Statement: Clinical practice guidelines for PTSD provide recommendations for enrolling patients in evidence-based psychotherapy (EBP). Unfortunately, uptake and engagement in EBPs for PTSD remain low and strategies are needed to optimize treatment outcomes. This seminar will provide contemporary data about factors that predict who will engage in and those most likely to experience a sub-optimal response from treatment. The focus of the seminar will be on optimizing strategies to enhance successful participation in treatment for PTSD.
Learning Objectives:
- Understand who is likely to receive evidence-based treatment in VA
- Understand who is likely to complete an adequate dose of evidence-based treatment
- Describe the factors that put Veterans at risk of suboptimal response to evidence-based treatment
March 20, 2024: The ongoing legacy of COVID: Relationships between COVID-19 infection, prior history of traumatic stress, and the risk of long term symptoms (aka Long COVID)
Rebecca Hendrickson, PhD
Purpose Statement: The purpose of this continuing education lecture is to explore the relationships between COVID-19 infection, a history of traumatic stress, and the heightened risk of experiencing long-term symptoms. Emerging research findings will be discussed to provide healthcare professionals with a comprehensive understanding of how past traumatic experiences may intersect with COVID-19 infection to exacerbate the likelihood and severity of persistent symptoms. Attendees will learn strategies for addressing the overlap between persistent physical symptoms related to PTSD and COVID-19.
Learning Objectives:
- Understand the potential common underlying mechanisms by which traumatic stress and physiologic stress may both cause lasting changes in physiology.
- Understand the potential for a history of traumatic stress to increase the risk of persistent symptoms after a subsequent stressor
- Feel comfortable talking about the potential overlap between persistent physical symptoms related to PTSD and physical symptoms related to COVID-19 infection in a way that is validating of patients experiences, and recognizes the complex interplay between central and peripheral stress-response systems.
March 6, 2024: Adapting and pilot testing a family-involved intervention to increase initiation and completion of evidence-based psychotherapy for PTSD
Megan Shepherd-Banigan, PhD
Purpose Statement: Evidence-based psychotherapies (EBPs) for PTSD are highly effective, yet uptake and adherence to these interventions is low. Incorporating family into PTSD treatment may be one strategy to improve engagement and treatment completion. This seminar will describe the process of adapting a behavioral intervention to include family members in PTSD treatment and provide early results from this intervention. This session will provide clinicians with strategies to effectively implement family-involved interventions for PTSD, ultimately with the goal of improving outcomes for veterans with PTSD.
Learning Objectives:
- To state the potential importance of family involvement in Veteran mental health care.
- To describe the process of adapting a behavioral intervention to test in a clinical setting.
- To consider the advantages and disadvantages to family involved interventions for Veterans with PTSD
February 21, 2024: Racism, Systemic Oppression, and Health Disparities: How to engage in effective allyship and build anti-racist practice
Sarah Súñiga, PhD
Malinda Trujillo, PhD
Purpose Statement: As a healthcare provider, it is imperative we understand how systemic oppression manifests as health disparities and our role in maintaining these disparities. Being an effective ally and engaging in anti-racism requires significant self-reflection, vulnerability, humility, equity, and familiarity with power and privilege. During this seminar, the speakers will explore and define racism, race-based trauma, systemic oppression, and health disparities. The session will explore steps and skills for becoming an effective and conscious ally as a healthcare provider, as well as anti-racism skills and resources.
Course Learning Objectives:
1. Define racism, race based trauma, and systemic oppression and their impact on veterans of color.
2. Define health disparities and their impact on veterans of color.
3. Identify skills and resources for becoming an ally within healthcare systems.
January 17, 2024: CogSMART / Compensatory Cognitive Training for Veterans with Mental Health Conditions
Elizabeth W Twamley, PhD
Purpose Statement: Compensatory Cognitive Training (CCT) is an evidence-based treatment designed to improve cognitive functioning and quality of life for Veterans who experienced mild traumatic brain injury (mTBI). Emerging data suggest CCT may also improve cognitive functioning among veterans with PTSD and other mental health conditions. This lecture will provide an overview of compensatory and restorative interventions to improve cognitive functioning in people with psychiatric disorders, mild TBI history, and mild cognitive impairment related to aging.
Course Learning Objectives:
- Describe compensatory and restorative interventions to improve cognition in people with psychiatric disorders.
- List domains of cognitive functioning targeted in Compensatory Cognitive Training.
- Describe how to link cognitive strategies with individual rehabilitation goals.
December 20, 2023: Women veterans at acute risk for suicide: Care needs and preferences
Lauren Denneson, PhD
Purpose Statement: There are gender differences in the acute care needs of veterans at risk of suicide, though little empirical information is available to guide care. The purpose of this lecture is to review the care needs of women veterans at acute risk of suicide. Participants will gain insights and strategies for customizing mental health treatment to enhance intervention effectiveness. The lecture will address gender-specific risk factors, enabling clinicians to recognize and navigate challenges unique to gender. Additionally, participants will understand the dynamic nature of risk and resilience over time, examining how these factors evolve in both women and men experiencing acute suicide risk.
Course Learning Objectives:
- Describe the stated care preferences of women veterans at acute risk of suicide
- List risk factors for suicide that are more common among acute-risk women than men
- Describe how risk and resilience changes over time in acute-risk women and men
December 6, 2023: Barriers to the Use of Medications for Opioid Use Disorder and How to Overcome Them
Jessica Wyse, PhD
Purpose Statement: Opioid use disorder (OUD) remains a crisis in the United States and among veterans treated in Veterans Health Administration (VHA). For those with OUD, receipt of medications for opioid use disorder (MOUD) is associated with substantial improvements in morbidity and mortality. Unfortunately, many patients with OUD do not receive treatment and those who do often discontinue MOUD at high rates. This seminar will provide contemporary data about the multifaceted barriers that hinder engagement and retention in treatment for OUD. Through a critical examination of the social, systemic, and individual impediments, this lecture will provide healthcare professionals with a comprehensive understanding of OUD treatment challenges and provide evidence-based strategies designed to bolster treatment engagement and retention.
Course Learning Objectives:
- Understand the benefits of medications for the treatment of opioid use disorder
- Define barriers to engagement and retention in treatment for opioid use disorder
- Identify strategies to improve opioid use disorder treatment engagement
November 15, 2023: Who to, when to, and how to address Obstructive Sleep Apnea (OSA) among Veterans: Strategies for mental health clinicians
Yeilim Cho, MD
Purpose Statement: Obstructive sleep apnea (OSA) occurs in one-third to one-half of veterans with mental health conditions. This seminar will provide mental health clinicians with a comprehensive understanding of OSA and its clinical implications. During this session, participants will gain insights into the epidemiology, risk factors, and clinical manifestations of OSA, enabling them to identify and assess OSA in their clients. This will emphasize the bidirectional relationship between OSA and conditions such as depression, anxiety, and cognitive impairments. By equipping mental health professionals with the knowledge and tools to diagnose and treat OSA, this lecture aims to enhance the overall well-being and treatment outcomes of their patients.
Course Learning Objectives:
- Understand the high prevalence of sleep-disordered breathing in Veteran
- Understand whom and when to treat OSA in Veteran
- Understand current challenges and strategies in treating OSA in Veteran
November 1, 2023: Cultural aspects of PTSD assessment and treatment
James Boehnlein, MD
Purpose Statement: By identifying and reviewing the influence of cultural factors on the experience, expression, and recovery from PTSD, this session seeks to empower mental health clinicians with culturally sensitive and informed strategies for assessment and treatment. Through a review of diverse cultural perspectives and coping mechanisms, attendees will acquire the knowledge and skills needed to conduct more effective assessments, develop tailored treatment plans, and foster trustful therapeutic alliances with veterans and refugees. This lecture aims to enhance the cultural competence of mental health practitioners, promoting more inclusive and culturally responsive approaches to PTSD care.
Course Learning Objectives:
- List the most important elements of a comprehensive cultural formulation
- Identify the role of culture in PTSD clinical assessment among diverse populations, including refugees and Veterans
- Discuss how culture influences PTSD treatment and outcomes
October 18, 2023: Addressing loneliness and social disconnectedness as a transdiagnostic risk factor
Lisham Ashrafioun, PhD
Purpose Statement: This lecture will explore the impact of loneliness and social disconnection as transdiagnostic risk factors for mental health impairment. By examining the pervasive impact of these psychosocial risk factors across various mental health conditions, this session aims to equip clinicians with a comprehensive understanding of the relationship between loneliness, social isolation, and mental well-being. This lecture will provide contemporary data on behavioral interventions and practical strategies to equip attendees with the skills necessary to identify, address, and mitigate the adverse effects of loneliness, ultimately fostering more effective approaches to mental health care.
Course Learning Objectives:
1. Define loneliness and social isolation
2. Understand the relationship between loneliness and behavioral and physical health conditions
3. Identify cognitive-behavioral approaches of addressing loneliness
October 4, 2023: Neuropsychiatric aspects of Long COVID
Jordan Anderson, DO
Purpose Statement: Those who have been infected with COVD-19 can experience long-term effects from their infection, known as Long COVID. The purpose of this lecture is to provide mental health clinicians with a specialized and comprehensive understanding of the neuropsychiatric aspects of Long COVID. By focusing on the intersection of mental health and neurology in the context of post-acute COVD-19 syndrome, this presentation aims to equip attendees with the knowledge and tools necessary to assess and effectively treat the unique neuropsychiatric challenges experienced by individuals with Long COVID.
Course Learning Objectives:
- Review common neuropsychiatric symptoms of Long COVID
- Identify comorbidities of Long COVID and their impact on treatment
- Discuss management strategies for Long COVID care
Sign up for email updates or access your subscriber preferences: https://public.govdelivery.com/accounts/USVHAVISN20/subscriber/new.
Use of these Materials and Finding VA Health Care
Please note that the health care information provided in these materials is for educational purposes only. It does not replace the role of a medical practitioner for advice on care and treatment. If you are looking for professional medical care, find your local VA healthcare center by using the VA Facilities Locator & Directory. This page may contain links that will take you outside of the Department of Veterans Affairs website. VA does not endorse and is not responsible for the content of the linked websites.
VA Web Disclaimers
Disclaimer of Endorsement: Reference herein to any specific commercial products, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government, and shall not be used for advertising or product endorsement purposes.
Disclaimer of Hyperlinks: The appearance of external hyperlinks does not constitute endorsement by the Department of Veterans Affairs of the linked websites, or the information, products or services contained therein. For other than authorized VA activities, the Department does not exercise any editorial control over the information you may find at these locations. All links are provided with the intent of meeting the mission of the Department and the VA website. Please let us know about existing external links which you believe are inappropriate and about specific additional external links which you believe ought to be included.
Disclaimer of Liability: With respect to documents available from this server, neither the United States Government nor any of its employees, makes any warranty, express or implied, including the warranties of merchantability and fitness for a particular purpose, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights.
Reference from this web page or from any of the information services sponsored by the VA to any non-governmental entity, product, service or information does not constitute an endorsement or recommendation by the VA or any of its employees. We are not responsible for the content of any "off-site" web pages referenced from this server.
Disclaimer: The sharing of any non-VA information does not constitute an endorsement of products or services on the part of the VA.
![]()
VA Regional Offices
 The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
Find out if you can get VA health care as a Veteran
The following four categories of Veterans are not required to enroll but are urged to do so to permit better planning of health resources:
- Veterans with a service-connected (SC) disability rated at 50% or more.
- Veterans seeking care for a disability the military determined was incurred or aggravated in the line of duty, but which VA has not yet rated, within 12 months of discharge.
- Veterans seeking care for a SC disability only or under a special treatment authority.
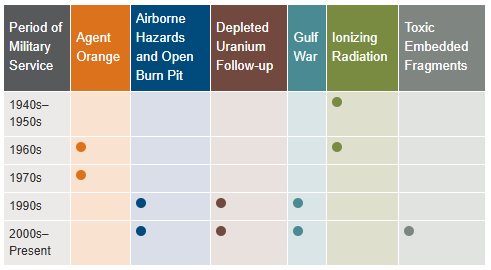
- Veterans seeking health registry examinations. VA’s health registry evaluation is a free, voluntary medical assessment for Veterans who may have been exposed to certain environmental hazards during military service. The evaluations alert Veterans to possible long-term health problems that may be related to exposure to specific environmental hazards during their military service. VA has established several health registries to track and monitor the health of specific groups of Veterans. You may be eligible to participate in one or more of these health registries: Agent Orange Registry, Airborne Hazards and Open Burn Pit Registry, Gulf War Registry (includes Operations Iraqi Freedom and New Dawn), Ionizing Radiation Registry, Depleted Uranium Follow-Up Program, and Toxic Embedded Fragment Surveillance Center. Use the chart below to help determine your eligibility.
Find out how to apply for VA health care benefits as a Veteran or service member. For other mental health services, contact a VA medical center for information on eligibility and treatment options.
Community Care (Mission Act)
The MISSION Act became law in 2018, bringing the VA’s previous Veterans Choice Program to an end and establishing the Community Care Program. VA provides health care for Veterans from providers in your local community outside of VA. Veterans may be eligible to receive care from a community provider when VA cannot provide the care needed. This care is provided on behalf of and paid for by VA. Community care is also available to Veterans based on certain conditions and eligibility requirements, and in consideration of a Veteran’s specific needs and circumstances. VA offers urgent care services to eligible Veterans at in-network urgent care clinics to treat minor injuries and illnesses that are not life-threatening, such as colds, strep throat, sprained muscles, and skin and ear infections. Community care must be first authorized by VA before a Veteran can receive care from a community provider.
Vet Centers in VISN 20
 Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Alaska
| Anchorage Vet Center (Anchorage, AK) | Fairbanks Vet Center (Fairbanks, AK) |
| Kenai Vet Center Outstation (Soldotna, AK) | Wasilla Vet Center (Wasilla, AK) |
Idaho
| Boise Vet Center (Boise, ID) | East Idaho Vet Center (Idaho Falls, ID) |
Oregon
| Central Oregon Vet Center (Bend, OR) | Eugene Vet Center (Eugene, OR) |
| Grants Pass Vet Center (Grants Pass, OR) | Portland, OR Vet Center (Portland, OR) |
| Salem Vet Center (Salem, OR) |
Washington
Plan your trip to VA
 In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
VCS operates over 200 Patriot Stores in Veterans Administration (VA) Medical Centers nationwide. Many of our stores have been recently updated and expanded to provide our customers with a modern, clean and comfortable shopping experience. Our stores welcome our customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations.
The Patriot Cafe is the best place in the VA Medical Center to enjoy delicious, freshly prepared breakfast or lunch served hot or cold each weekday. Providing Veterans, their families, VA employees, volunteers and visitors a place to relax and enjoy a meal or take-out for their convenience. With a wide variety of food from traditional comfort food, specialized menu selections and a large assortment of healthy choices; there is something for everyone's taste buds.
Hospital Service Directory
To find out whether there is a van near you use the Disabled American Veterans (DAV) Hospital Service Coordinator Directory to contact your nearest HSC for information or assistance. Please remember that the DAV Transportation Network is staffed by volunteers; therefore, it is unable to cover every community. The vans are driven by volunteers, and the rides coordinated by more than 133 Hospital Service Coordinators around the country. Our nation’s heroes travel around the globe to protect our freedoms—it’s only right that we return their dedication. Volunteering to drive a Vet ensures that even those living remotely from VA hospitals can make their appointments and never go without the treatment they need. Learn more about the DAV transportation network through the VISN 20 NewsFlash Resources section.
 Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
VA Puget Sound Health Care System (VAPSHCS) serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. Veterans Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA Outpatient Clinics and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
VA Portland Health Care System (VAPORHCS) serves Veterans in Oregon and Southwest Washington with two main divisions: Portland VA Medical Center and Vancouver VA Medical Center. Veterans Medical Centers are also located in Roseburg, White City, and Vancouver, Washington. VA Outpatient Clinics and Vet Centers are located in Astoria, Bend, Boardman, Brookings, Eugene, Fairview, Grants Pass, Hines, Hillsboro, Klamath Falls, LaGrande, Lincoln City, Newport, Portland, Salem, The Dalles, and West Linn.