MIRECC / CoE
2021 VISN 20 MIRECC Staff Research Articles and Presentations
VISN 20 MIRECC Staff Research Articles and Presentations
The findings of NW MIRECC research are disseminated through MIRECC Presents, lectures and presentations, and publications. Below is a list of publications and presentations by VISN 20 NW MIRECC researchers and fellowship program faculty that were published in 2021.
Andrea, S. B., Gilbert, T. A., Morasco, B., Saha, S., & Carlson, K. F. (2021). Factors related to prescription drug monitoring program queries for veterans receiving long-term opioid therapy. Pain Medicine, 22, 1548-1558.
Arditte Hall, K., DeLane, S., Anderson, G., Lago, T., Shor, R., Wang, X., Rasmusson, A. M., & Pineles, S. L. (2021). Plasma gamma-aminobutyric acid (GABA) levels and posttraumatic stress disorder symptoms in trauma-exposed women: a preliminary report. Psychopharmacology, 238, 1541-1552. doi:10.1007/s00213-021-05785-z
Asher, D., Belay, E., Bigio, E., Brandner, S., Brubaker, S., Caughey, B., Clark, B., Damon, I., Diamond, M., Freund, M., Hyman, B., Jucker, M., Keene, C., Lieberman, A., Mackiewicz, M., Montine, T., Morgello, S., Phelps, C., Safar, J., Schneider, J., Schonberger, L., Sigurdson, C., Silverberg, N., Trojanowski, J., & Frosch, M. (2020). Risk of Transmissibility From Neurodegenerative Disease-Associated Proteins: Experimental Knowns and Unknowns. Journal of Neuropathology and Experimental Neurology, 79 (11), 1141-1146. doi:10.1093/jnen/nlaa109
Barnes, N., Ahern, G., Becamel, C., Bockaert, J., Camilleri, M., Chaumont-Dubel, S., Claeysen, S., Cunningham, K., Fone, K., Gershon, M., Di Giovanni, G., Goodfellow, N., Halberstadt, A., Hartley, R., Hassaine, G., Herrick-Davis, K., Hovius, R., Lacivita, E., Lambe, E., Leopoldo, M., Levy, F., Lummis, S., Marin, P., Maroteaux, L., McCreary, A., Nelson, D., Neumaier, J. F., Newman-Tancredi, A., Nury, H., Roberts, A., Roth, B., Roumier, A., Sanger, G., Teitler, M., Sharp, T., Villalón, C., Vogel, H., Watts, S., & Hoyer, D. (2020). International Union of Basic and Clinical Pharmacology. CX. Classification of Receptors for 5-hydroxytryptamine; Pharmacology and Function. Pharmacological Reviews, 73 (1), 310-520. doi:10.1124/pr.118.015552
Bieniek, K., Cairns, N., Crary, J., Dickson, D., Folkerth, R., Keene, C., Litvan, I., Perl, D., Stein, T., Vonsattel, J., Stewart, W., Dams-O’Connor, K., Gordon, W., Tripodis, Y., Alvarez, V., Mez, J., Alosco, M., McKee, A., Babcock, D., Bellgowan, P., Crane, P., Edlow, B., Huber, B., Kiernan, P., & Koroshetz, W. (2021). The Second NINDS/NIBIB Consensus Meeting to Define Neuropathological Criteria for the Diagnosis of Chronic Traumatic Encephalopathy. Journal of Neuropathology and Experimental Neurology, 80 (3), 210-219. doi:10.1093/jnen/nlab001
Bird, E., Piccirillo, M., Garcia, N., Blais, R., & Campbell, S. (2021). Relationship Between Posttraumatic Stress Disorder and Sexual Difficulties: A Systematic Review of Veterans and Military Personnel. The Journal of Sexual Medicine, 18 (8), 1398-1426. doi:10.1016/j.jsxm.2021.05.011
Borsari, B., Li, Y., Tighe, J., Manuel, J. K., Gokbayrak, N. S., Delucchi, K., Morasco, B., Abadjian, L., Cohen, B. E., Baxley, C., & Seal, K. H. (2021). A pilot trial of collaborative care with motivational interviewing to reduce opioid risk and improve chronic pain management. Addiction, 116, 2387-2397.
Bourassa, K. J., Hendrickson, R. C., Reger, G. M., & Norr, A. M. (2021). Posttraumatic Stress Disorder Treatment Effects on Cardiovascular Physiology: a Systematic Review and Agenda for Future Research. J Trauma Stress. 34(2):384-393, 34(2), 384-393.
Bowen, S., Dingle, T., Laue, C., Mallik, D., & Somohano, V. (2021). Overlaying Buddhist and behaviorist lenses to better understand and address human suffering. Spirituality in Clinical Practice, 8(4), 281–289. doi:10.1037/scp0000275
Brawman-Mintzer, O., Tang, X. C., Bizien, M., Harvey, P. D., Arciniegas, D. B., Raskind, M. A., Johnson-Greene, L., Martineau, R. J., Hamner, M., Rodriguez-Suarez, M., Jorge, R. E., McGarity, S., Wortzel, H., Wei, Y., Sindowski, T., Mintzer, J., Kindy, A. Z., Donovan, K., & Reda, D. (2021). Rivastigmine Transdermal Patch Treatment for Moderate to Severe Cognitive Impairment in Veterans with Traumatic Brain Injury (RiVET Study): a Randomized Clinical Trial. Journal of Neurotrauma. doi: 10.1089/neu.2020.7146
Brett, B., Kramer, M., Whyte, J., McCrea, M., Stein, M., Giacino, J., Sherer, M., Markowitz, A., Manley, G., Nelson, L., Adeoye, O., Badjatia, N., Boase, K., Barber, J., Bodien, Y., Bullock, M., Chesnut, R., Corrigan, J., Crawford, K., Diaz-Arrastia, R., Dikmen, S., Duhaime, A., Ellenbogen, R., Feeser, V., Ferguson, A., Foreman, B., Gardner, R., Gaudette, E., Gonzalez, L., Gopinath, S., Gullapalli, R., Hemphill, J., Hotz, G., Jain, S., Keene, C., Korley, F., Kramer, J., Kreitzer, N., Levin, H., Lindsell, C., Machamer, J., Madden, C., Martin, A., McAllister, T., Merchant, R., Mukherjee, P., Ngwenya, L., Noel, F., Okonkwo, D., Palacios, E., Puccio, A., Rabinowitz, M., Robertson, C., Rosand, J., Sander, A., Satris, G., Schnyer, D., Seabury, S., Taylor, S., Temkin, N., Toga, A., Valadka, A., Vassar, M., Wang, K., Yue, J., Yuh, E., & Zafonte, R. (2021). Latent Profile Analysis of Neuropsychiatric Symptoms and Cognitive Function of Adults 2 Weeks After Traumatic Brain Injury. JAMA Network Open, 4 (3), e213467. doi:10.1001/jamanetworkopen.2021.3467
Bryson, W. C., Morasco, B., Cotton, B. P., & Thielke, S. M. (2021). Cannabis use and nonfatal opioid overdose among patients enrolled in methadone maintenance treatment. Substance Use & Misuse, 56, 697-703.
Carter, S. P., Campbell, S. B., Wee, J. Y., Law, K. C., Lehavot, K., Simpson, T., & Reger, M. A. (2022). Suicide Attempts Among Racial and Ethnic Groups in a Nationally Representative Sample. Journal of racial and ethnic health disparities, 9(5), 1783–1793. doi:10.1007/s40615-021-01115-3.
Caulfield, N., Martin, R., Norr, A. M., & Capron, D. (2021). The Association Between Posttraumatic Stress Symptoms and Anxiety Sensitivity in a College Sample. Psychological Reports, 124 (4), 1539-1558. doi:10.1177/0033294120948227
Christensen, V., Nugent, S. M., Ayers, C., Morasco, B., & Kansagara, D. (2021). A qualitative study of VHA clinicians’ knowledge and perspectives on cannabis for medical purposes. Family Practice, 38, 479-483.
Cohen, D., Sullivan, K., McNeil, R., Klimas, N., McNeil, R., Ashford, W., Bested, A., Bunker, J., Cheema, A., Cohen, D., Cook, D. G., Cournoyer, J., Craddock, T., Golier, J., Hardie, A., Helmer, D., Lindheimer, J., Lloyd, P., Kerr, K., Krengel, M., Nadkarni, S., Nugent, S., Paris, B., Reinhard, M., Rumm, P., Schneiderman, A., Sims, K., Steele, L., Turner, M., Sullivan, K., Abdullah, L., Abreu, M., Abu-Donia, M., Aenlle, K., Arocho, J., Balbin, E., Baraniuk, J., Block, K., Block, M., DeBeer, B., Engdahl, B., Filipov, N., Fletcher, M., Kalasinsky, V., Kokkotou, E., Lidie, K., Little, D., Loging, W., Morris, M., Nathanson, L., Nichols, M., Pasinetti, G., Shungu, D., Waziry, P., VanLeeuwen, J., Younger, J., & Klimas, N. (2021). A common language for Gulf War Illness (GWI) research studies: GWI common data elements. Life Sciences. doi:10.1016/j.lfs.2021.119818
Daniels, R., Clouston, S., Hall, C., Anderson, K., Bennett, D., Bromet, E., Calvert, G., Carreón, T., DeKosky, S., Diminich, E., Finch, C., Gandy, S., Kreisl, W., Kritikos, M., Kubale, T., Mielke, M., Peskind, E. R., Raskind, M. A., Richards, M., Sano, M., Santiago-Colón, A., Sloan, R., Spiro, A., Vasdev, N., Luft, B., & Reissman, D. (2021). A Workshop on Cognitive Aging and Impairment in the 9/11-Exposed Population. International Journal of Environmental Research and Public Health, 18 (2), 681. doi:10.3390/ijerph18020681
Davis, M., Wheelock, V., Talman, L., Latimer, C., Vicars, B., Lin, A., Jayadev, S., & Bird, T. (2021). Subdural Hematoma as a Serious Complication of Huntington’s Disease: An Observational Study. Journal of Huntington's Disease, Online ahead of print, 1-6. doi:10.3233/JHD-210478
Gajera, C., Fernandez, R., Montine, K., Fox, E., Mrdjen, D., Postupna, N., Keene, C., Bendall, S., & Montine, T. (2021). Mass-tag barcoding for multiplexed analysis of human synaptosomes and other anuclear events. Cytometry Part A. doi:10.1002/cyto.a.24340
Gauthreaux, K., Bonnett, T. A., Besser, L. M., Brenowitz, W. D., Teylan, M., Mock, C., Chen, Y. C., KCG, C., Keene, C., Zhou, X. H., & Kukull, W. A. (2020). Concordance of Clinical Alzheimer Diagnosis and Neuropathological Features at Autopsy. Journal of Neuropathology and Experimental Neurology, 79(5), 465-473. doi: 10.1093/jnen/nlaa014.
Goodman, J., & Iliff, J. J. (2020). Vasomotor influences on glymphatic-lymphatic coupling and solute trafficking in the central nervous system. Journal of Cerebral Blood Flow and Metabolism, 40 (8), 1724-1734. doi:10.1177/0271678X19874134
Gozt, A., Hellewell, S., Thorne, J., Thomas, E., Buhagiar, F., Markovic, S., Van Houselt, A., Ring, A., Arendts, G., Smedley, B., Van Schalkwyk, S., Brooks, P., Iliff, J. J., Celenza, A., Mukherjee, A., Xu, D., Robinson, S., Honeybul, S., Cowen, G., Licari, M., Bynevelt, M., Pestell, C., Fatovich, D., & Fitzgerald, M. (2021). Predicting outcome following mild traumatic brain injury: protocol for the longitudinal, prospective, observational Concussion Recovery (CREST) cohort study. BMJ Open, 11 (5), e046460. doi:10.1136/bmjopen-2020-046460
Gramlich, M., Smolenski, D., Norr, A. M., Rothbaum, B., Rizzo, A., Andrasik, F., Fantelli, E., & Reger, G. (2021). Psychophysiology during exposure to trauma memories: Comparative effects of virtual reality and imaginal exposure for posttraumatic stress disorder. Depression and Anxiety, 38 (6), 626-638. doi:10.1002/da.23141
Hampel, H., Shaw, L., Aisen, P., Chen, C., Lleó, A., Iwatsubo, T., Iwata, A., Yamada, M., Ikeuchi, T., Jia, J., Wang, H., Teunissen, C., Peskind, E. R., Blennow, K., Cummings, J., & Vergallo, A. (2021). State-of-the-art of lumbar puncture and its place in the journey of patients with Alzheimer's disease. Alzheimer's & Dementia. doi:10.1002/alz.12372
Hendrickson, R. C. (2021). Assessing Risk When Everyone's Afraid: The Challenge of Seeing Health Care Workers as People When Our Need for Them Is So Great. Narrative Inquiry in Bioethics, 11 (1), 32-35. doi:10.1353/nib.2021.0011
Hendrickson, R. C., Millard, S., Pagulayan, K. F., Peskind, E. R., & Raskind, M. A. (2021). The Relative Effects of Prazosin on Individual PTSD Symptoms: Evidence for Pathophysiologically-Related Clustering. Chronic Stress, 5, 247054702097978. doi:10.1177/2470547020979780
Henriksen, J., Kolognizak, T., Houghton, T., Cherne, S., Zhen, D., Cimino, P., Latimer, C., Scherpelz, K., Yoda, R., Alpers, C., Chhieng, D., Keene, C., & Gonzalez-Cuyar, L. (2020). Rapid Validation of Telepathology by an Academic Neuropathology Practice During the COVID-19 Pandemic. Archives of Pathology and Laboratory Medicine, 144 (11), 1311-1320. doi:10.5858/arpa.2020-0372-SA
Hoerster, K. D., Tanksley, L., Sulayman, N., Bondzie, J., Brier, M., Damschroder, L., Coggeshall, S., Houseknecht, D., Hunter-Merrill, R., Monty, G., Saelens, B., Sayre, G., Simpson, T. L., Wong, E., & Nelson, K. (2021). Testing a tailored weight management program for veterans with PTSD: The MOVE! + UP randomized controlled trial. Contemporary Clinical Trials, 107, 106487. doi:10.1016/j.cct.2021.106487
Holmer, H. K., Gilbert, T. A., Ashraf, A. J., O’Neil, M., & Carlson, K. F. (2021). Opioid and Sedative-Hypnotic Prescriptions among Post-9/11 Veteran VA Users Nationwide with Traumatic Brain Injury. Journal of Head Trauma and Rehabilitation. 36(5): 354-363, 36(5), 354-363.
Hong, Z., Tian, C., Stewart, T., Aro, P., Soltys, D., Bercow, M., Sheng, L., Borden, K., Khrisat, T., Pan, C., Zabetian, C., Peskind, E. R., Quinn, J., Montine, T., Aasly, J., Shi, M., & Zhang, J. (2021). Development of a Sensitive Diagnostic Assay for Parkinson Disease Quantifying a-Synuclein–Containing Extracellular Vesicles. Neurology, 96 (18), e2332-e2345. doi:10.1212/WNL.0000000000011853
Jansson, D., & Iliff, J. J. (2021). Woes with flows under pressure. Brain Communications, 3 (2), fcab094. doi:10.1093/braincomms/fcab094
Kalmbach, B., Hodge, R., Jorstad, N., Owen, S., de Frates, R., Yanny, A., Dalley, R., Mallory, M., Graybuck, L., Radaelli, C., Keene, C., Gwinn, R., Silbergeld, D., Cobbs, C., Ojemann, J., Ko, A., Patel, A., Ellenbogen, R., Bakken, T., Daigle, T., Dee, N., Lee, B., McGraw, M., Nicovich, P., Smith, K., Sorensen, S., Tasic, B., Zeng, H., Koch, C., Lein, E., & Ting, J. (2021). Signature morpho-electric, transcriptomic, and dendritic properties of human layer 5 neocortical pyramidal neurons. Neuron, 109 (18), 2914-2927.e5. doi:10.1016/j.neuron.2021.08.030
Katz, D., Bernick, C., Dodick, D., Mez, J., Mariani, M., Adler, C., Alosco, M., Balcer, L., Banks, S., Barr, W., Brody, D., Cantu, R., Dams-O'Connor, K., Geda, Y., Jordan, B., McAllister, T., Peskind, E. R., Petersen, R., Wethe, J., Zafonte, R., Foley, É., Babcock, D., Koroshetz, W., Tripodis, Y., McKee, A., Shenton, M., Cummings, J., Reiman, E., & Stern, R. (2021). National Institute of Neurological Disorders and Stroke Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome. Neurology, 96(18), 848-863. doi:10.1212/WNL.0000000000011850
Kersch, C., Claunch, C., Ambady, P., Bucher, E., Schwartz, D., Barajas, R., Iliff, J. J., Risom, T., Heiser, L., Muldoon, L., Korkola, J., Gray, J., & Neuwelt, E. (2020). Transcriptional signatures in histologic structures within glioblastoma tumors may predict personalized drug sensitivity and survival. Neuro-Oncology Advances, 2(1), vdaa093. doi:10.1093/noajnl/vdaa093
Korvatska, O., Kiianitsa, K., Ratushny, A., Matsushita, M., Beeman, N., Chien, W., Satoh, J., Dorschner, M., Keene, C., Bammler, T., Bird, T., & Raskind, W. (2020). Triggering Receptor Expressed on Myeloid Cell 2 R47H Exacerbates Immune Response in Alzheimer’s Disease Brain. Frontiers in Immunology, 11, 559342. doi:10.3389/fimmu.2020.559342
Kow, R., Strovas, T., McMillan, P., Jacobi, A., Behlke, M., Saxton, A., Latimer, C., Keene, C., & Kraemer, B. C. (2021). Distinct Poly(A) nucleases have differential impact on sut-2 dependent tauopathy phenotypes. Neurobiology of Disease, 147, 105148. doi:10.1016/j.nbd.2020.105148
Krukowski, K., Nolan, A., Frias, E., Boone, M., Ureta, G., Grue, K., Paladini, M., Elizarraras, E., Delgado, L., Bernales, S., Walter, P., & Rosi, S. (2020). Small molecule cognitive enhancer reverses age-related memory decline in mice. eLife, 9, e62048. doi:10.7554/eLife.62048
Kunkle, B., Schmidt, M., Klein, H., Naj, A., Hamilton-Nelson, K., Larson, E., Evans, D., De Jager, P., Crane, P., Buxbaum, J., Ertekin-Taner, N., Barnes, L., Fallin, M., Manly, J., Go, R., Obisesan, T., Kamboh, M., Bennett, D., Hall, K., Goate, A., Foroud, T., Martin, E., Wang, L., Byrd, G., Farrer, L., Haines, J., Schellenberg, G., Mayeux, R., Pericak-Vance, M., Reitz, C., Abner, E., Adams, P., Albin, R., Apostolova, L., Arnold, S., Atwood, C., Baldwin, C., Barber, R., Barral, S., Beach, T., Becker, J., Beecham, G., Bigio, E., Bird, T., Blacker, D., Boeve, B., Bowen, J., Boxer, A., Burke, J., Burns, J., Cairns, N., Cao, C., Carlsson, C., Carney, R., Carrasquillo, M., Cribbs, D., Cruchaga, C., Dick, M., Dickson, D., Doody, R., Duara, R., Faber, K., Fairchild, T., Fallon, K., Fardo, D., Farlow, M., Ferris, S., Frosch, M., Galasko, D., Gearing, M., Geschwind, D., Ghetti, B., Gilbert, J., Green, R., Growdon, J., Hakonarson, H., Hamilton, R., Hardy, J., Harrell, L., Honig, L., Huebinger, R., Huentelman, M., Hulette, C., Jarvik, G., Jin, L., Karydas, A., Katz, M., Kauwe, J., Keene, C., Kim, R., Kramer, J., Lah, J., Leung, Y., Li, G., Lieberman, A., Lipton, R., Lyketsos, C., Malamon, J., Marson, D., Martiniuk, F., Masliah, E., McCormick, W., McCurry, S., McDavid, A., McDonough, S., McKee, A., Mesulam, M., Miller, B., Miller, C., Montine, T., Mukherjee, S., Myers, A., O’Bryant, S., Olichney, J., Parisi, J., Peskind, E. R., Pierce, A., Poon, W., Potter, H., Qu, L., Quinn, J., Raj, A., Raskind, M., Reisberg, B., Reisch, J., Ringman, J., Roberson, E., Rogaeva, E., Rosen, H., Royall, D., Sager, M., Schneider, J., Schneider, L., Seeley, W., Small, S., Sonnen, J., Spina, S., St George-Hyslop, P., Stern, R., Tanzi, R., Troncoso, J., Tsuang, D., Valladares, O., Van Deerlin, V., Vardarajan, B., Vinters, H., Vonsattel, J., Weintraub, S., Welsh-Bohmer, K., Wilhelmsen, K., Williamson, J., Wingo, T., Woltjer, R., Wu, C., Younkin, S., Yu, L., Yu, C., Zhao, Y., Graff-Radford, N., Martinez, I., Ayodele, T., Logue, M. W., Cantwell, L., Jean-Francois, M., Kuzma, A., Adams, L., Vance, J., Cuccaro, M., Chung, J., Mez, J., Lunetta, K., Jun, G., Lopez, O., Hendrie, H., Reiman, E., Kowall, N., Leverenz, J., Small, S., Levey, A., Golde, T., Saykin, A., Starks, T., Albert, M., Hyman, B., Petersen, R., Sano, M., Wisniewski, T., Vassar, R., Kaye, J., Henderson, V., DeCarli, C., LaFerla, F., Brewer, J., Miller, B., Swerdlow, R., Van Eldik, L., Paulson, H., Trojanowski, J., Chui, H., Rosenberg, R., Craft, S., Grabowski, T., Asthana, S., Morris, J., Strittmatter, S., & Kukull, W. (2021). Novel Alzheimer disease risk loci and pathways in African American individuals using the African Genome Resources Panel. JAMA Neurology, 78, 102-113. doi:10.1001/jamaneurol.2020.3536
Latimer, C., & Liachko, N. (2021). Tau and TDP-43 synergy: a novel therapeutic target for sporadic late-onset Alzheimer’s disease. GeroScience, Online ahead of print., Online ahead of print.. doi:10.1007/s11357-021-00407-0
Latimer, C., Lucot, K., Keene, C., Cholerton, B., & Montine, T. (2021). Genetic Insights into Alzheimer's Disease. Annual Review of Pathology: Mechanisms of Disease, 16 (1), 351-376. doi:10.1146/annurev-pathmechdis-012419-032551
Lauterborn, J., Scaduto, P., Cox, C., Schulmann, A., Lynch, G., Gall, C., Keene, C., & Limon, A. (2021). Increased excitatory to inhibitory synaptic ratio in parietal cortex samples from individuals with Alzheimer’s disease. Nature Communications, 12 (1), 2603. doi:10.1038/s41467-021-22742-8
Lehavot, K., Millard, S., Thomas, R., Yantsides, K., Upham, M., Beckman, K., Hamilton, A., Sadler, A., Litz, B., & Simpson, T. L. (2021). A randomized trial of an online, coach-assisted self-management PTSD intervention tailored for women veterans. Journal of Consulting and Clinical Psychology, 89 (2), 134-142. doi:10.1037/ccp0000556
Levin, H., Temkin, N., Barber, J., Nelson, L., Robertson, C., Brennan, J., Stein, M., Yue, J., Giacino, J., McCrea, M., Diaz-Arrastia, R., Mukherjee, P., Okonkwo, D., Boase, K., Markowitz, A., Bodien, Y., Taylor, S., Vassar, M., Manley, G., Adeoye, O., Badjatia, N., Bullock, M., Chesnut, R., Corrigan, J., Crawford, K., Dikmen, S., Duhaime, A., Ellenbogen, R., Feeser, V., Ferguson, A., Foreman, B., Gardner, R., Gaudette, E., Gonzalez, L., Gopinath, S., Gullapalli, R., Hemphill, J., Hotz, G., Jain, S., Keene, C., Korley, F., Kramer, J., Kreitzer, N., Lindsell, C., Machamer, J., Madden, C., Martin, A., McAllister, T., Merchant, R., Nolan, A., Ngwenya, L., Noel, F., Palacios, E., Puccio, A., Rabinowitz, M., Rosand, J., Sander, A., Satris, G., Schnyer, D., Seabury, S., Sun, X., Toga, A., Valadka, A., Wang, K., Yuh, E., & Zafonte, R. (2021). Association of Sex and Age With Mild Traumatic Brain Injury–Related Symptoms: A TRACK-TBI Study. JAMA Network Open, 4 (4), e213046. doi:10.1001/jamanetworkopen.2021.3046
Levinstein, M., Coffey, K. R., Marx, R., Lesiak, A., & Neumaier, J. F. (2020). Stress induces divergent gene expression among lateral habenula efferent pathways. Neurobiology of Stress, 13, 100268. doi:10.1016/j.ynstr.2020.100268
Li, G., Jankowski, A., Shofer, J., Roggenkamp, H., Tsuang, D., Peskind, E. R., & Raskind, M. A. (2020). Cognitive trajectory changes in African American veterans with combat PTSD. Alzheimer's & Dementia, 16 (S6), e047359. doi:10.1002/alz.047359
Livingston, N., Simpson, T. L., Lehavot, K., Ameral, V., Brief, D., Enggasser, J., Litwack, S., Helmuth, E., Roy, M., Rosenbloom, D., & Keane, T. M. (2021). Differential alcohol treatment response by gender following use of VetChange. Drug and Alcohol Dependence, 221, 108552. doi:10.1016/j.drugalcdep.2021.108552
Lusardi, T., Sandau, U., Sakhanenko, N., Baker, S., Wiedrick, J., Lapidus, J., Raskind, M. A., Li, G., Peskind, E. R., Galas, D., Quinn, J., & Saugstad, J. (2021). Cerebrospinal Fluid MicroRNA Changes in Cognitively Normal Veterans With a History of Deployment-Associated Mild Traumatic Brain Injury. Frontiers in Neuroscience. doi:10.3389/fnins.2021.720778
Magaletta, P. R., & Morasco, B. (2021). Perspectives on opioid misuse from public service psychology: an introduction. Psychological Services, 18, 285-286.
Mallik, D., Kaplan, J., Somohano, V., Bergman, A., & Bowen, S. (2021). Examining the Role of Craving, Mindfulness, and Psychological Flexibility in a Sample of Individuals with Substance Use Disorder. Substance Use & Misuse, 56 (6), 782-786. doi:10.1080/10826084.2021.1899220
McCrea, M., Giacino, J., Barber, J., Temkin, N., Nelson, L., Levin, H., Dikmen, S., Stein, M., Bodien, Y., Boase, K., Taylor, S., Vassar, M., Mukherjee, P., Robertson, C., Diaz-Arrastia, R., Okonkwo, D., Markowitz, A., Manley, G., Adeoye, O., Badjatia, N., Bullock, M., Chesnut, R., Corrigan, J., Crawford, K., Duhaime, A., Ellenbogen, R., Feeser, V., Ferguson, A., Foreman, B., Gardner, R., Gaudette, E., Goldman, D., Gonzalez, L., Gopinath, S., Gullapalli, R., Hemphill, J., Hotz, G., Jain, S., Keene, C., Korley, F., Kramer, J., Kreitzer, N., Lindsell, C., Machamer, J., Madden, C., Martin, A., McAllister, T., Merchant, R., Ngwenya, L., Noel, F., Nolan, A., Palacios, E., Perl, D., Puccio, A., Rabinowitz, M., Rosand, J., Sander, A., Satris, G., Schnyer, D., Seabury, S., Sherer, M., Toga, A., Valadka, A., Wang, K., Yue, J., Yuh, E., & Zafonte, R. (2021). Functional Outcomes Over the First Year After Moderate to Severe Traumatic Brain Injury in the Prospective, Longitudinal TRACK-TBI Study. JAMA Neurology, 78 (8), 982. doi:10.1001/jamaneurol.2021.2043
McMillan, P., Strovas, T., Baum, M., Mitchell, B., Eck, R., Hendricks, N., Wheeler, J., Latimer, C., Keene, C., & Kraemer, B. C. (2021). Pathological tau drives ectopic nuclear speckle scaffold protein SRRM2 accumulation in neuron cytoplasm in Alzheimer’s disease. Acta Neuropathologica Communications, 9 (1), 117. doi:10.1186/s40478-021-01219-1
McMillan, P., Wheeler, J., Gatlin, R., Taylor, L., Strovas, T., Baum, M., Bird, T., Latimer, C., Keene, C., Kraemer, B. C., & Liachko, N. F. (2020). Adult onset pan-neuronal human tau tubulin kinase 1 expression causes severe cerebellar neurodegeneration in mice. Acta Neuropathologica Communications, 8 (1), 200. doi:10.1186/s40478-020-01073-7
Meabon, J., Cook, D. G., Yagi, M., Terry, G., Cross, D., Muzi, M., Pagulayan, K. F., Logsdon, A., Schindler, A., Ghai, V., Wang, K., Fallen, S., Zhou, Y., Kim, T., Lee, I., Banks, W., Carlson, E., Mayer, C., Hendrickson, R. C., Raskind, M. A., Marshall, D., Perl, D., Keene, C., & Peskind, E. R. (2020). Chronic elevation of plasma vascular endothelial growth factor-A (VEGF-A) is associated with a history of blast exposure. Journal of the Neurological Sciences, 417, 117049. doi:10.1016/j.jns.2020.117049
Mich, J., Graybuck, L., Hess, E., Mahoney, J., Kojima, Y., Ding, Y., Somasundaram, S., Miller, J., Kalmbach, B., Radaelli, C., Gore, B., Weed, N., Omstead, V., Bishaw, Y., Shapovalova, N., Martinez, R., Fong, O., Yao, S., Mortrud, M., Chong, P., Loftus, L., Bertagnolli, D., Goldy, J., Casper, T., Dee, N., Opitz-Araya, X., Cetin, A., Smith, K., Gwinn, R., Cobbs, C., Ko, A., Ojemann, J., Keene, C., Silbergeld, D., Sunkin, S., Gradinaru, V., Horwitz, G., Zeng, H., Tasic, B., Lein, E., Ting, J., & Levi, B. (2021). Functional enhancer elements drive subclass-selective expression from mouse to primate neocortex. Cell Reports, 34 (13), 108754. doi:10.1016/j.celrep.2021.108754
Michailidou, D., Chung, S., Andrews, J., Starkebaum, G., Chew, F., & Latimer, C. (2021). An Unusual Case of Proximal Limb Muscle Weakness. Arthritis & Rheumatology, 73 (3), 541-541. doi:10.1002/art.41626
Miller, M., Williams, R., Pagulayan, K. F., Barber, J., Ehde, D., & Hoffman, J. (2021). Correlates of sleep disturbance in Veterans with traumatic brain injury and chronic pain: A cross-sectional study. Disability and Health Journal. doi:10.1016/j.dhjo.2021.101203
Morasco, B., Iacocca, M. O., Lovejoy, T. I., Dobscha, S. K., Deyo, R. A., Cavese, J. A., Hyde, S., & Yarborough, B...J...H... (2021). Utility of the Pain Medication Questionnaire to predict aberrant urine drug tests: Results from a longitudinal cohort study. Psychological Services, 18, 319-327.
Mukherjee, S., Mez, J., Trittschuh, E., Saykin, A., Gibbons, L., Fardo, D., Wessels, M., Bauman, J., Moore, M., Choi, S., Gross, A., Rich, J., Louden, D., Sanders, R., Grabowski, T., Bird, T., McCurry, S., Snitz, B., Kamboh, M., Lopez, O., De Jager, P., Bennett, D., Keene, C., Larson, E., & Crane, P. (2020). Genetic data and cognitively defined late-onset Alzheimer’s disease subgroups. Molecular Psychiatry, 25 (11), 2942-2951. doi:10.1038/s41380-018-0298-8
Niemela, G., & Terry, G. (2021). Contribution of Fatty Acid Amide Hydrolase to Alcohol Use Disorder: A Systematic Review. Cannabis and Cannabinoid Research, 6 (2), 105-118. doi:10.1089/can.2020.0158
Nolan, A., Petersen, C., Iacono, D., Mac Donald, C., Mukherjee, P., van der Kouwe, A., Jain, S., Stevens, A., Diamond, B., Wang, R., Markowitz, A., Fischl, B., Perl, D., Manley, G., Keene, C., Diaz-Arrastia, R., Edlow, B., Adeoye, O., Badjatia, N., Boase, K., Barber, J., Bodien, Y., Bullock, M., Chesnut, R., Corrigan, J., Crawford, K., Dikmen, S., Duhaime, A., Ellenbogen, R., Feeser, V., Ferguson, A., Foreman, B., Gardner, R., Gaudette, E., Giacino, J., Goldman, D., Gonzalez, L., Gopinath, S., Gullapalli, R., Hemphill, J., Hotz, G., Korley, F., Kramer, J., Kreitzer, N., Levin, H., Lindsell, C., Machamer, J., Madden, C., Martin, A., McAllister, T., McCrea, M., Merchant, R., Nelson, L., Ngwenya, L., Noel, F., Okonkwo, D., Palacios, E., Puccio, A., Rabinowitz, M., Robertson, C., Rosand, J., Sander, A., Satris, G., Schnyer, D., Seabury, S., Sherer, M., Stein, M., Taylor, S., Temkin, N., Toga, A., Valadka, A., Vassar, M., Vespa, P., Wang, K., Yue, J., Yuh, E., & Zafonte, R. (2021). Tractography-Pathology Correlations in Traumatic Brain Injury: A TRACK-TBI Study. Journal of Neurotrauma. Advance online publication. doi:10.1089/neu.2020.7373
O’Bryan, E., McLeish, A., Norr, A. M., Ely, S., Bass, Z., Davies, C., Capron, D., Schmidt, N., & Mano, K. (2021). A randomized controlled trial evaluating the efficacy of a brief computerized anxiety sensitivity reduction intervention for health anxiety. Journal of Anxiety Disorders, 82, 102425. doi:10.1016/j.janxdis.2021.102425
O'Neil, M. E., Klyce, D. W., Pogoda, T. K., Cifu, D. X., Eggleston, B. E., Cameron, D. C., Wilde, E. A., Walker, W. C., & Carlson, K. F. (2021). Associations Among PTSD and Postconcussive Symptoms in the Long-Term Impact of Military-Relevant Brain Injury Consortium-Chronic Effects of Neurotrauma Consortium Prospective, Longitudinal Study Cohort. The Journal of head trauma rehabilitation, 36(6), E363–E372. Doi:10.1097/HTR.0000000000000665
O'Neil, M., Cameron, D., Shirley, K., Sano, E., Twamley, E. W., Williams, R., Turner, A., Pagulayan, K. F., Roost, M., Jak, A. J., Storzbach, D., & Huckans, M. (2021). Change in Learning and Memory Partially Mediates Effects of Compensatory Cognitive Training on Self-Reported Cognitive Symptoms. Journal of Head Trauma Rehabilitation, 36 (6), 429-436. doi:10.1097/HTR.0000000000000662
Piantino, J., Schwartz, D., Luther, M., Newgard, C., Silbert, L., Raskind, M. A., Pagulayan, K. F., Kleinhans, N., Iliff, J. J., & Peskind, E. R. (2021). Link between mild traumatic brain injury, poor sleep, and MRI-visible perivascular spaces in Veterans. Journal of Neurotrauma. doi:10.1089/neu.2020.7447
Postupna, N., Rose, S., Gibbons, L., Coleman, N., Hellstern, L., Ritchie, K., Wilson, A., Cudaback, E., Li, X., Melief, E., Beller, A., Miller, J., Nolan, A., Marshall, D., Walker, R., Montine, T., Larson, E., Crane, P., Ellenbogen, R., Lein, E., Dams-O'Connor, K., & Keene, C. (2021). The Delayed Neuropathological Consequences of Traumatic Brain Injury in a Community-Based Sample. Frontiers in Neurology, 12, 624696. doi:10.3389/fneur.2021.624696
Prater, K., Latimer, C., & Jayadev, S. (2021). Glial TDP-43 and TDP-43 induced glial pathology, focus on neurodegenerative proteinopathy syndromes. Glia, Online ahead of print, Online ahead of print. doi:10.1002/glia.24096
Reger, G., Harned, M., Stevens, E., Porter, S., Nguyen, J., & Norr, A. M. (2021). Mobile applications may be the future of veteran mental health support but do veterans know yet? A survey of app knowledge and use. Psychological Services, xx, xx. doi:10.1037/ser0000562
Reger, G., Norr, A. M., Gramlich, M., & Buchman, J. (2021). Virtual Standardized Patients for Mental Health Education. Current Psychiatry Reports, 23(9), 57. doi:10.1007/s11920-021-01273-5
Reger, G., Norr, A. M., Rizzo, A., Sylvers, P., Peltan, J., Fischer, D., Trimmer, M., Porter, S., Gant, P., & Baer, J. (2020). Virtual Standardized Patients vs Academic Training for Learning Motivational Interviewing Skills in the US Department of Veterans Affairs and the US Military. JAMA Network Open, 3 (10), e2017348. doi:10.1001/jamanetworkopen.2020.17348
Richard, E. L., Althouse, A. D., Arnsten, J. H., Bulls, H. W., Kansagara, D., Kerbag, M. N., Luchius, C., Lipsey, D., Morasco, B., Nugent, S. M., Merlin, J. S., & Starrels, J. L. (2021). How medical are states’ medical cannabis policies?: Proposing a standardized scale. International Journal of Drug Policy, 94, 103202.
Salman, M., Kitchen, P., Iliff, J. J., & Bill, R. (2021). Aquaporin 4 and glymphatic flow have central roles in brain fluid homeostasis. Nature Reviews Neuroscience, 22 (10), 650-651. doi:10.1038/s41583-021-00514-z
Schindler, A., Terry, G., Wolden-Hanson, T., Cline, M., Park, M., Lee, J., Yagi, M., Meabon, J., Peskind, E. R., Raskind, M. A., Phillips, P., & Cook, D. G. (2021). Repetitive Blast Promotes Chronic Aversion to Neutral Cues Encountered in the Peri-Blast Environment. Journal of Neurotrauma. doi:10.1089/neu.2020.7061
Seal, K. H., Becker, W. C., Murphy, J. L., Purcell, N., Denneson, L. M., Morasco, B., Martin, A. M., Reddy, K., Van Iseghem, T., Krebs, E. E., Painter, J. M., Hagedorn, H., Pyne, J. M., Hixon, J., Maguen, S., Neylan, R. C., Borsari, B., DeRonne, B., Gibson, C., Matthias, M. S., Frank, J. W., Krishnaswamy, A., Li, Y., Bertenthal, D., Chan, A., Nunez, A., & McCamish, N. (2020). wHOPE: a pragmatic trial comparing whole health team vs primary care group education to promote nonpharmacological strategies to improve pain, functioning, and quality of life in Veterans--Rationale, methods, and implementation. Pain Medicine, 21(Suppl. 2), s91-s99. doi:10.1093/pm/pnaa366
Shaffer, R., Li, G., Adar, S., Dirk Keene, C., Latimer, C., Crane, P., Larson, E., Kaufman, J., Carone, M., & Sheppard, L. (2021). Fine Particulate Matter and Markers of Alzheimer’s Disease Neuropathology at Autopsy in a Community-Based Cohort. Journal of Alzheimer's Disease, 79 (4), 1761-1773. doi:10.3233/JAD-201005
Shaffer, R., Sheppard, L., Peskind, E. R., Zhang, J., Adar, S. D., & Li, G. (2021). Fine Particulate Matter Exposure and Cerebrospinal Fluid Markers of Vascular Injury (pp. 135-145). Amsterdam: IOS Press.
Sheppard, D., Rau, H., Werhane, M., Peskind, E. R., & Pagulayan, K. F. (2021). A-128 Intraindividual Neurocognitive Variability Is Associated with Poorer Prospective Memory in OEF/OIF/OND Veterans with Comorbid Mild Traumatic Brain Injury History and Current Posttraumatic Stress Disorder. Archives of Clinical Neuropsychology, 36 (6), 1179-1179. doi:10.1093/arclin/acab062.146
Smith, D., Dollé, J., Ameen-Ali, K., Bretzin, A., Cortes, E., Crary, J., Dams-O’Connor, K., Diaz-Arrastia, R., Edlow, B., Folkerth, R., Hazrati, L., Hinds, S., Iacono, D., Johnson, V., Keene, C., Kofler, J., Kovacs, G., Lee, E., Manley, G., Meaney, D., Montine, T., Okonkwo, D., Perl, D., Trojanowski, J., Wiebe, D., Yaffe, K., McCabe, T., & Stewart, W. (2021). COllaborative Neuropathology NEtwork Characterizing ouTcomes of TBI (CONNECT-TBI). Acta Neuropathologica Communications, 9 (1), 32. doi:10.1186/s40478-021-01122-9
Somohano, V., Shank, T., Manuel, J., Mallik, D., Rehder, K., & Bowen, S. (2021). The Role of Pretreatment Expectancy on Substance Use Outcomes in Women Mandated to Mindfulness-Based Relapse Prevention. The Journal of Alternative and Complementary Medicine. doi:10.1089/acm.2021.0123
Spina, S., La Joie, R., Petersen, C., Nolan, A., Cuevas, D., Cosme, C., Hepker, M., Hwang, J., Miller, Z., Huang, E., Karydas, A., Grant, H., Boxer, A., Gorno-Tempini, M., Rosen, H., Kramer, J., Miller, B., Seeley, W., Rabinovici, G., & Grinberg, L. (2021). Comorbid neuropathological diagnoses in early versus late-onset Alzheimer’s disease. Brain, 144 (7), 2186-2198. doi:10.1093/brain/awab099
Stein, M., Yuh, E., Jain, S., Okonkwo, D., Mac Donald, C., Levin, H., Giacino, J., Dikmen, S., Vassar, M., Diaz-Arrastia, R., Robertson, C., Nelson, L., McCrea, M., Sun, X., Temkin, N., Taylor, S., Markowitz, A., Manley, G., Mukherjee, P., Adeoye, O., Badjatia, N., Boase, K., Barber, J., Bodien, Y., Bullock, M., Chesnut, R., Corrigan, J., Crawford, K., Duhaime, A., Ellenbogen, R., Feeser, V., Ferguson, A., Foreman, B., Gardner, R., Gaudette, E., Goldman, D., Gonzalez, L., Gopinath, S., Gullapalli, R., Hemphill, J., Hotz, G., Jain, S., Keene, C., Korley, F., Kramer, J., Kreitzer, N., Lindsell, C., Machamer, J., Madden, C., Martin, A., McAllister, T., Merchant, R., Ngwenya, L., Noel, F., Nolan, A., Palacios, E., Perl, D., Puccio, A., Rabinowitz, M., Robertson, C., Rosand, J., Sander, A., Satris, G., Schnyer, D., Seabury, S., Toga, A., Valadka, A., Vespa, P., Wang, K., Yue, J., & Zafonte, R. (2021). Smaller Regional Brain Volumes Predict Posttraumatic Stress Disorder at 3 Months After Mild Traumatic Brain Injury. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 6 (3), 352-359. doi:10.1016/j.bpsc.2020.10.008
Stevens, E., Bourassa, K., Norr, A. M., & Reger, G. (2021). Posttraumatic Stress Disorder Symptom Cluster Structure in Prolonged Exposure Therapy and Virtual Reality Exposure. Journal of Traumatic Stress, 34 (2), 287-297. doi:10.1002/jts.22602
Uretsky, M., Gibbons, L., Mukherjee, S., Trittschuh, E., Fardo, D., Boyle, P., Keene, C., Saykin, A., Crane, P., Schneider, J., & Mez, J. (2021). Longitudinal cognitive performance of Alzheimer's disease neuropathological subtypes. Alzheimer's & Dementia: Translational Research & Clinical Interventions, 7 (1), e12201. doi:10.1002/trc2.12201
Wang, C., Shao, C., Zhang, L., Siedlak, S., Meabon, J., Peskind, E. R., Lu, Y., Wang, W., Perry, G., Cook, D. G., & Zhu, X. (2021). Oxidative Stress Signaling in Blast TBI-Induced Tau Phosphorylation. Antioxidants, 10 (6), 955. doi:10.3390/antiox10060955
Wang, M., Ray, L., Tanaka, K., Iliff, J. J., & Heys, J. (2021). Varying perivascular astroglial endfoot dimensions along the vascular tree maintain perivascular-interstitial flux through the cortical mantle. Glia, 69(3), 715-728. doi:10.1002/glia.23923
Wang, X., Xie, H., Chen, T., Cotton, A., Salminen, L., Logue, M. W., Clarke-Rubright, E., Wall, J., Dennis, E., O’Leary, B., Abdallah, C., Andrew, E., Baugh, L., Bomyea, J., Bruce, S., Bryant, R., Choi, K., Daniels, J., Davenport, N., Davidson, R., DeBellis, M., deRoon-Cassini, T., Disner, S., Fani, N., Fercho, K., Fitzgerald, J., Forster, G., Frijling, J., Geuze, E., Gomaa, H., Gordon, E. M., Grupe, D., Harpaz-Rotem, I., Haswell, C., Herzog, J., Hofmann, D., Hollifield, M., Hosseini, B., Hudson, A., Ipser, J., Jahanshad, N., Jovanovic, T., Kaufman, M., King, A., Koch, S., Koerte, I., Korgaonkar, M., Krystal, J. H., Larson, C., Lebois, L., Levy, I., Li, G., Magnotta, V., Manthey, A., May, G. J., McLaughlin, K., Mueller, S., Nawijn, L., Nelson, S. M., Neria, Y., Nitschke, J., Olff, M., Olson, E., Peverill, M., Luan Phan, K., Rashid, F., Ressler, K., Rosso, I., Sambrook, K., Schmahl, C., Shenton, M., Sierk, A., Simons, J., Simons, R., Sponheim, S., Stein, M., Stein, D., Stevens, J., Straube, T., Suarez-Jimenez, B., Tamburrino, M., Thomopoulos, S., van der Wee, N., van der Werff, S., van Erp, T., van Rooij, S., van Zuiden, M., Varkevisser, T., Veltman, D., Vermeiren, R., Walter, H., Wang, L., Zhu, Y., Zhu, X., Thompson, P., Morey, R., & Liberzon, I. (2021). Cortical volume abnormalities in posttraumatic stress disorder: an ENIGMA-psychiatric genomics consortium PTSD workgroup mega-analysis. Molecular Psychiatry, 26 (8), 4331-4343. doi:10.1038/s41380-020-00967-1
Wang, X., Zhou, X., Uberseder, B., Lee, J., Latimer, C., Furdui, C., Keene, C., Montine, T., Register, T., Craft, S., Shively, C., & Ma, T. (2021). Isoform-specific dysregulation of AMP-activated protein kinase signaling in a non-human primate model of Alzheimer's disease. Neurobiology of Disease, 158, 105463. doi:10.1016/j.nbd.2021.105463
Webster, J., Grabowski, T., Madhyastha, T., Gibbons, L., Keene, C., & Latimer, C. (2021). Leveraging Neuroimaging Tools to Assess Precision and Accuracy in an Alzheimer’s Disease Neuropathologic Sampling Protocol. Frontiers in Neuroscience, 15, 693242. doi:10.3389/fnins.2021.693242
Williams, J., Nieblas-Bedolla, E., Feroze, A., Young, C., Temkin, N., Giacino, J., Okonkwo, D., Manley, G., Barber, J., Durfy, S., Markowitz, A., Yuh, E., Mukherjee, P., Mac Donald, C., Adeoye, O., Badjatia, N., Boase, K., Bodien, Y., Bullock, M., Chesnut, R., Corrigan, J., Crawford, K., Diaz-Arrastia, R., Dikmen, S., Duhaime, A., Ellenbogen, R., Feeser, V., Ferguson, A., Foreman, B., Gardner, R., Gaudette, E., Goldman, D., Gonzalez, L., Gopinath, S., Gullapalli, R., Hemphill, J., Hotz, G., Jain, S., Keene, C., Korley, F., Kramer, J., Kreitzer, N., Levin, H., Lindsell, C., Machamer, J., Madden, C., Martin, A., McAllister, T., McCrea, M., Merchant, R., Nelson, L., Ngwenya, L., Noel, F., Nolan, A., Palacios, E., Perl, D., Puccio, A., Rabinowitz, M., Robertson, C., Rosand, J., Sander, A., Satris, G., Schnyer, D., Seabury, S., Stein, M., Taylor, S., Toga, A., Valadka, A., Vassar, M., Vespa, P., Wang, K., Yue, J., & Zafonte, R. (2021). Prognostic Value of Hemorrhagic Brainstem Injury on Early Computed Tomography: A TRACK-TBI Study. Neurocritical Care. doi:10.1007/s12028-021-01263-8
Wu, S., Furlan, S., Mihalas, A., Kaya-Okur, H., Feroze, A., Emerson, S., Zheng, Y., Carson, K., Cimino, P., Keene, C., Sarthy, J., Gottardo, R., Ahmad, K., Henikoff, S., & Patel, A. (2021). Single-cell CUT&Tag analysis of chromatin modifications in differentiation and tumor progression. Nature Biotechnology, 39 (7), 819-824. doi:10.1038/s41587-021-00865-z
Wu, Z., Wang, Z., Liu, X., Zhang, Z., Gu, X., Yu, S., Keene, C., Cheng, L., & Ye, K. (2020). Traumatic brain injury triggers APP and Tau cleavage by delta-secretase, mediating Alzheimer’s disease pathology. Progress in Neurobiology, 185, 101730. doi:10.1016/j.pneurobio.2019.101730
Wyse, J., *Simmons, A., *Ramachandran, B., Dobscha, S. K., & Morasco, B. (2021). “I don’t mind doing what it takes to be safe.” Patient perspectives of urine drug testing for pain. Journal of General Internal Medicine, 36, 243-244.
Wyse, J., Lovejoy, J., Holloway, J., Morasco, B., Dobscha, S. K., Hagedorn, H., & Lovejoy, T. I. (2021). Patients’ perceptions of the pathways linking problematic substance use with chronic pain. Pain, 162, 787-793.
Yildiz, S., Lim, M., Sammi, M., Powers, K., Murchison, C., Iliff, J. J., & Rooney, W. (2021). 252 Non-Invasive Quantification of Human Brain Lactate Concentrations Across Sleep-Wake Cycles. Sleep, 44 (Supplement_2), A101-A102. doi:10.1093/sleep/zsab072.251
Zhang, F., Gannon, M., Chen, Y., Yan, S., Zhang, S., Feng, W., Tao, J., Sha, B., Liu, Z., Saito, T., Saido, T., Keene, C., Jiao, K., Roberson, E., Xu, H., & Wang, Q. (2020). ß-amyloid redirects norepinephrine signaling to activate the pathogenic GSK3ß/tau cascade. Science Translational Medicine, 12 (526), eaay6931. doi:10.1126/scitranslmed.aay6931
Zhang, W., Davis, C., Zeppenfeld, D., Golgotiu, K., Wang, X., Haveliwala, M., Hong, D., Li, Y., Wang, R., Iliff, J. J., & Alkayed, N. (2021). Role of endothelium-pericyte signaling in capillary blood flow response to neuronal activity. Journal of Cerebral Blood Flow and Metabolism, 41(8), 1873-1885. doi:10.1177/0271678X211007957
Sign up for email updates or access your subscriber preferences: https://public.govdelivery.com/accounts/USVHAVISN20/subscriber/new.
Use of these Materials and Finding VA Health Care
Please note that the health care information provided in these materials is for educational purposes only. It does not replace the role of a medical practitioner for advice on care and treatment. If you are looking for professional medical care, find your local VA healthcare center by using the VA Facilities Locator & Directory. This page may contain links that will take you outside of the Department of Veterans Affairs website. VA does not endorse and is not responsible for the content of the linked websites.
VA Web Disclaimers
Disclaimer of Endorsement: Reference herein to any specific commercial products, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government, and shall not be used for advertising or product endorsement purposes.
Disclaimer of Hyperlinks: The appearance of external hyperlinks does not constitute endorsement by the Department of Veterans Affairs of the linked websites, or the information, products or services contained therein. For other than authorized VA activities, the Department does not exercise any editorial control over the information you may find at these locations. All links are provided with the intent of meeting the mission of the Department and the VA website. Please let us know about existing external links which you believe are inappropriate and about specific additional external links which you believe ought to be included.
Disclaimer of Liability: With respect to documents available from this server, neither the United States Government nor any of its employees, makes any warranty, express or implied, including the warranties of merchantability and fitness for a particular purpose, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights.
Reference from this web page or from any of the information services sponsored by the VA to any non-governmental entity, product, service or information does not constitute an endorsement or recommendation by the VA or any of its employees. We are not responsible for the content of any "off-site" web pages referenced from this server.
Disclaimer: The sharing of any non-VA information does not constitute an endorsement of products or services on the part of the VA.
![]()
VA Regional Offices
 The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
Find out if you can get VA health care as a Veteran
The following four categories of Veterans are not required to enroll but are urged to do so to permit better planning of health resources:
- Veterans with a service-connected (SC) disability rated at 50% or more.
- Veterans seeking care for a disability the military determined was incurred or aggravated in the line of duty, but which VA has not yet rated, within 12 months of discharge.
- Veterans seeking care for a SC disability only or under a special treatment authority.
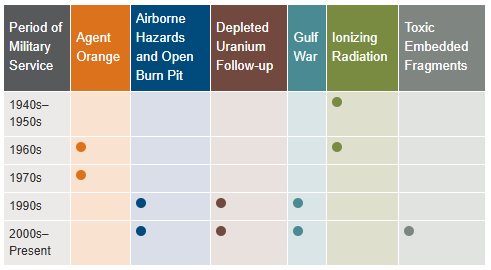
- Veterans seeking health registry examinations. VA’s health registry evaluation is a free, voluntary medical assessment for Veterans who may have been exposed to certain environmental hazards during military service. The evaluations alert Veterans to possible long-term health problems that may be related to exposure to specific environmental hazards during their military service. VA has established several health registries to track and monitor the health of specific groups of Veterans. You may be eligible to participate in one or more of these health registries: Agent Orange Registry, Airborne Hazards and Open Burn Pit Registry, Gulf War Registry (includes Operations Iraqi Freedom and New Dawn), Ionizing Radiation Registry, Depleted Uranium Follow-Up Program, and Toxic Embedded Fragment Surveillance Center. Use the chart below to help determine your eligibility.
Find out how to apply for VA health care benefits as a Veteran or service member. For other mental health services, contact a VA medical center for information on eligibility and treatment options.
Community Care (Mission Act)
The MISSION Act became law in 2018, bringing the VA’s previous Veterans Choice Program to an end and establishing the Community Care Program. VA provides health care for Veterans from providers in your local community outside of VA. Veterans may be eligible to receive care from a community provider when VA cannot provide the care needed. This care is provided on behalf of and paid for by VA. Community care is also available to Veterans based on certain conditions and eligibility requirements, and in consideration of a Veteran’s specific needs and circumstances. VA offers urgent care services to eligible Veterans at in-network urgent care clinics to treat minor injuries and illnesses that are not life-threatening, such as colds, strep throat, sprained muscles, and skin and ear infections. Community care must be first authorized by VA before a Veteran can receive care from a community provider.
Vet Centers in VISN 20
 Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Alaska
| Anchorage Vet Center (Anchorage, AK) | Fairbanks Vet Center (Fairbanks, AK) |
| Kenai Vet Center Outstation (Soldotna, AK) | Wasilla Vet Center (Wasilla, AK) |
Idaho
| Boise Vet Center (Boise, ID) | East Idaho Vet Center (Idaho Falls, ID) |
Oregon
| Central Oregon Vet Center (Bend, OR) | Eugene Vet Center (Eugene, OR) |
| Grants Pass Vet Center (Grants Pass, OR) | Portland, OR Vet Center (Portland, OR) |
| Salem Vet Center (Salem, OR) |
Washington
Plan your trip to VA
 In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
VCS operates over 200 Patriot Stores in Veterans Administration (VA) Medical Centers nationwide. Many of our stores have been recently updated and expanded to provide our customers with a modern, clean and comfortable shopping experience. Our stores welcome our customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations.
The Patriot Cafe is the best place in the VA Medical Center to enjoy delicious, freshly prepared breakfast or lunch served hot or cold each weekday. Providing Veterans, their families, VA employees, volunteers and visitors a place to relax and enjoy a meal or take-out for their convenience. With a wide variety of food from traditional comfort food, specialized menu selections and a large assortment of healthy choices; there is something for everyone's taste buds.
Hospital Service Directory
To find out whether there is a van near you use the Disabled American Veterans (DAV) Hospital Service Coordinator Directory to contact your nearest HSC for information or assistance. Please remember that the DAV Transportation Network is staffed by volunteers; therefore, it is unable to cover every community. The vans are driven by volunteers, and the rides coordinated by more than 133 Hospital Service Coordinators around the country. Our nation’s heroes travel around the globe to protect our freedoms—it’s only right that we return their dedication. Volunteering to drive a Vet ensures that even those living remotely from VA hospitals can make their appointments and never go without the treatment they need. Learn more about the DAV transportation network through the VISN 20 NewsFlash Resources section.
 Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
VA Puget Sound Health Care System (VAPSHCS) serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. Veterans Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA Outpatient Clinics and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
VA Portland Health Care System (VAPORHCS) serves Veterans in Oregon and Southwest Washington with two main divisions: Portland VA Medical Center and Vancouver VA Medical Center. Veterans Medical Centers are also located in Roseburg, White City, and Vancouver, Washington. VA Outpatient Clinics and Vet Centers are located in Astoria, Bend, Boardman, Brookings, Eugene, Fairview, Grants Pass, Hines, Hillsboro, Klamath Falls, LaGrande, Lincoln City, Newport, Portland, Salem, The Dalles, and West Linn.