MIRECC / CoE
2022 VISN 20 MIRECC Staff Research Articles and Presentations
VISN 20 MIRECC Staff Research Articles and Presentations
The findings of NW MIRECC research are disseminated through MIRECC Presents, lectures and presentations, and publications. Below is a list of publications and presentations by VISN 20 NW MIRECC researchers and fellowship program faculty that were published in 2022.
Adeniyi, P., Fopiano, K., Banine, F., Garcia, M., Gong, X., Keene, C., Sherman, L., Bagi, Z., & Back, S. (2022). Multispectral LEDs Eliminate Lipofuscin-Associated Autofluorescence for Immunohistochemistry and CD44 Variant Detection by in Situ Hybridization in Aging Human, non-Human Primate, and Murine Brain. ASN Neuro, 14, 175909142211231. doi:10.1177/17590914221123138
Alosco, M., Mariani, M., Adler, C., Balcer, L., Bernick, C., Au, R., Banks, S., Barr, W., Bouix, S., Cantu, R., Coleman, M., Dodick, D., Farrer, L., Geda, Y., Katz, D., Koerte, I., Kowall, N., Lin, A., Marcus, D., Marek, K., McClean, M., McKee, A., Mez, J., Palmisano, J., Peskind, E. R., Tripodis, Y., Turner, R., Wethe, J., Cummings, J., Reiman, E., Shenton, M., Stern, R., Adler, C., Alosco, M., Au, R., Balcer, L., Banks, S., Barr, W., Bernick, C., Bouix, S., Cantu, R., Chen, K., Coleman, M., Cummings, J., Dodick, D., Farrer, L., Fitzsimmons, J., Geda, Y., Goldberg, J., Helm, R., Johnson, K., Katz, D., Kirov, I., Koerte, I., Kowall, N., Lin, A., Lui, Y., Marcus, D., Marek, K., Mariani, M., Marmar, C., McClean, M., McKee, A., Mez, J., Miller, J., Palmisano, J., Pasternak, O., Peskind, E. R., Protas, H., Reiman, E., Ritter, A., Shenton, M., Stern, R., Su, Y., Tripodis, Y., Turner, R., Weller, J., & Wethe, J. (2021). Developing methods to detect and diagnose chronic traumatic encephalopathy during life: rationale, design, and methodology for the DIAGNOSE CTE Research Project. Alzheimer's Research and Therapy, 13 (1), 136. doi:10.1186/s13195-021-00872-x
Alosco, M., Su, Y., Stein, T., Protas, H., Cherry, J., Adler, C., Balcer, L., Bernick, C., Pulukuri, S., Abdolmohammadi, B., Coleman, M., Palmisano, J., Tripodis, Y., Mez, J., Rabinovici, G., Marek, K., Beach, T., Johnson, K., Huber, B., Koerte, I., Lin, A., Bouix, S., Cummings, J., Shenton, M., Reiman, E., McKee, A., Stern, R., Reiman, E., Su, Y., Chen, K., Protas, H., Boker, C., Alosco, M., Au, R., Cantu, R., Farrer, L., Helm, R., Katz, D., Kowall, N., Mez, J., Mercier, G., Otis, J., Stern, R., Weller, J., Simkin, I., Andino, A., Conneely, S., Diamond, C., Fagle, T., Haller, O., Hunt, T., Gullotti, N., Mariani, M., Mayville, B., McLaughlin, K., Nanna, M., Platt, T., Pulukuri, S., Rice, F., Sestak, M., McClean, M., Tripodis, Y., Annis, D., Chaisson, C., Dixon, D., Finney, C., Gallagher, K., Hartlage, K., Lu, J., Martin, B., Ojo, E., Palmisano, J., Pine, B., Ramachandran, J., Bouix, S., Fitzsimmons, J., Lin, A., Koerte, I., Pasternak, O., Shenton, M., Arcinieago, H., Billah, T., Bonke, E., Breedlove, K., Coello, E., Coleman, M., Jung, L., Liao, H., Loy, M., Rizzoni, E., Schultz, V., Silva, A., Vessey, B., Wiegand, T., Banks, S., Bernick, C., Miller, J., Ritter, A., Sabbagh, M., de la Cruz, R., Durant, J., Golceker, M., Harmon, N., Kaylegian, K., Long, R., Nance, C., Sandoval, P., Turner, R., Marek, K., Serrano, A., Adler, C., Dodick, D., Geda, Y., Wethe, J., Falk, B., Duffy, A., Howard, M., Montague, M., Osgood, T., Babcock, D., Bellgowan, P., Balcer, L., Barr, W., Goldberg, J., Wisniewski, T., Kirov, I., Lui, Y., Marmar, C., Hasanaj, L., Serrano, L., Al-Kharafi, A., George, A., Martin, S., Riley, E., Runge, W., Cummings, J., Peskind, E. R., Colasurdo, E., Marcus, D., Gurney, J., Greenwald, R., & Johnson, K. (2022). Associations between near end-of-life flortaucipir PET and postmortem CTE-related tau neuropathology in six former American football players. European Journal of Nuclear Medicine and Molecular Imaging. Advance online publication. doi:10.1007/s00259-022-05963-x
Ameen-Ali, K., Bretzin, A., Lee, E., Folkerth, R., Hazrati, L., Iacono, D., Keene, C., Kofler, J., Kovacs, G., Nolan, A., Perl, D., Priemer, D., Smith, D., Wiebe, D., Stewart, W., Al-Sarraj, S., Cortes, E., Crary, J., Dams-O’Connor, K., Diaz-Arrastia, R., Dollé, J., Edlow, B., Fischl, B., Hinds, C., Johnson, V., Manley, G., Meaney, D., Okonkwo, D., Schneider, A., Schneider, J., Troakes, C., Trojanowski, J., van der Kouwe, A., & Yaffe, K. (2022). Detection of astrocytic tau pathology facilitates recognition of chronic traumatic encephalopathy neuropathologic change. Acta Neuropathologica Communications, 10 (1), 1-50. doi:10.1186/s40478-022-01353-4
Bagi, Z., Kroenke, C., Fopiano, K., Tian, Y., Filosa, J., Sherman, L., Larson, E., Keene, C., Degener O’Brien, K., Adeniyi, P., & Back, S. (2022). Association of cerebral microvascular dysfunction and white matter injury in Alzheimer’s disease. GeroScience. Advance online publication. doi:10.1007/s11357-022-00585-5
Bakken, T., Jorstad, N., Hu, Q., Lake, B., Tian, W., Kalmbach, B., Crow, M., Hodge, R., Krienen, F., Sorensen, S., Eggermont, J., Yao, Z., Aevermann, B., Aldridge, A., Bartlett, A., Bertagnolli, D., Casper, T., Castanon, R., Crichton, K., Daigle, T., Dalley, R., Dee, N., Dembrow, N., Diep, D., Ding, S., Dong, W., Fang, R., Fischer, S., Goldman, M., Goldy, J., Graybuck, L., Herb, B., Hou, X., Kancherla, J., Kroll, M., Lathia, K., van Lew, B., Li, Y., Liu, C., Liu, H., Lucero, J., Mahurkar, A., McMillen, D., Miller, J., Moussa, M., Nery, J., Nicovich, P., Niu, S., Orvis, J., Osteen, J., Owen, S., Palmer, C., Pham, T., Plongthongkum, N., Poirion, O., Reed, N., Rimorin, C., Rivkin, A., Romanow, W., Sedeño-Cortés, A., Siletti, K., Somasundaram, S., Sulc, J., Tieu, M., Torkelson, A., Tung, H., Wang, X., Xie, F., Yanny, A., Zhang, R., Ament, S., Behrens, M., Bravo, H., Chun, J., Dobin, A., Gillis, J., Hertzano, R., Hof, P., Höllt, T., Horwitz, G., Keene, C., Kharchenko, P., Ko, A., Lelieveldt, B., Luo, C., Mukamel, E., Pinto-Duarte, A., Preissl, S., Regev, A., Ren, B., Scheuermann, R., Smith, K., Spain, W., White, O., Koch, C., Hawrylycz, M., Tasic, B., Macosko, E., McCarroll, S., Ting, J., Zeng, H., Zhang, K., Feng, G., Ecker, J., Linnarsson, S., & Lein, E. (2021). Comparative cellular analysis of motor cortex in human, marmoset and mouse. Nature, 598 (7879), 111-119. doi:10.1038/s41586-021-03465-8
Balba, N., McBride, A., Callahan, M., Mist, S., Jones, K., Butler, M., Lim, M., & Heinricher, M. (2022). Photosensitivity Is Associated with Chronic Pain following Traumatic Brain Injury. Journal of Neurotrauma, 39 (17-18), 1183-1194. doi:10.1089/neu.2022.0019
Baskin, B., Lee, S., Skillen, E., Wong, K., Rau, H., Hendrickson, R. C., Pagulayan, K. F., Raskind, M. A., Peskind, E. R., Phillips, P., Cook, D. G., & Schindler, A. (2021). Repetitive Blast Exposure Increases Appetitive Motivation and Behavioral Inflexibility in Male Mice. Frontiers in Behavioral Neuroscience, 15, 792648. doi:10.3389/fnbeh.2021.792648
Berg, J., Sorensen, S., Ting, J., Miller, J., Chartrand, T., Buchin, A., Bakken, T., Budzillo, A., Dee, N., Ding, S., Gouwens, N., Hodge, R., Kalmbach, B., Lee, C., Lee, B., Alfiler, L., Baker, K., Barkan, E., Beller, A., Berry, K., Bertagnolli, D., Bickley, K., Bomben, J., Braun, T., Brouner, K., Casper, T., Chong, P., Crichton, K., Dalley, R., de Frates, R., Desta, T., Lee, S., D’Orazi, F., Dotson, N., Egdorf, T., Enstrom, R., Farrell, C., Feng, D., Fong, O., Furdan, S., Galakhova, A., Gamlin, C., Gary, A., Glandon, A., Goldy, J., Gorham, M., Goriounova, N., Gratiy, S., Graybuck, L., Gu, H., Hadley, K., Hansen, N., Heistek, T., Henry, A., Heyer, D., Hill, D., Hill, C., Hupp, M., Jarsky, T., Kebede, S., Keene, L., Kim, L., Kim, M., Kroll, M., Latimer, C., Levi, B., Link, K., Mallory, M., Mann, R., Marshall, D., Maxwell, M., McGraw, M., McMillen, D., Melief, E., Mertens, E., Mezei, L., Mihut, N., Mok, S., Molnar, G., Mukora, A., Ng, L., Ngo, K., Nicovich, P., Nyhus, J., Olah, G., Oldre, A., Omstead, V., Ozsvar, A., Park, D., Peng, H., Pham, T., Pom, C., Potekhina, L., Rajanbabu, R., Ransford, S., Reid, D., Rimorin, C., Ruiz, A., Sandman, D., Sulc, J., Sunkin, S., Szafer, A., Szemenyei, V., Thomsen, E., Tieu, M., Torkelson, A., Trinh, J., Tung, H., Wakeman, W., Waleboer, F., Ward, K., Wilbers, R., Williams, G., Yao, Z., Yoon, J., Anastassiou, C., Arkhipov, A., Barzo, P., Bernard, A., Cobbs, C., de Witt Hamer, P., Ellenbogen, R., Esposito, L., Ferreira, M., Gwinn, R., Hawrylycz, M., Hof, P., Idema, S., Jones, A., Keene, C., Ko, A., Murphy, G., Ng, L., Ojemann, J., Patel, A., Phillips, J., Silbergeld, D., Smith, K., Tasic, B., Yuste, R., Segev, I., de Kock, C., Mansvelder, H., Tamas, G., Zeng, H., Koch, C., & Lein, E. (2021). Human neocortical expansion involves glutamatergic neuron diversification. Nature, 598 (7879), 151-158. doi:10.1038/s41586-021-03813-8
Boase, K., Machamer, J., Temkin, N., Dikmen, S., Wilson, L., Nelson, L., Barber, J., Bodien, Y., Giacino, J., Markowitz, A., McCrea, M., Satris, G., Stein, M., Taylor, S., Manley, G., Adeoye, O., Bullock, M., Corrigan, J., Diaz-Arrastia, R., Ellenbogen, R., Feeser, V., Ferguson, A., Gardner, R., Goldman, D., Gopinath, S., Hemphill, J., Keene, C., Korley, F., Kramer, J., Kreitzer, N., Levin, H., Lindsell, C., Madden, C., Martin, A., McAllister, T., Merchant, R., Mukherjee, P., Ngwenya, L., Noel, F., Nolan, A., Okonkwo, D., Palacios, E., Perl, D., Puccio, A., Rabinowitz, M., Robertson, C., Rosand, J., Sander, A., Schnyer, D., Seabury, S., Sherer, M., Toga, A., Valadka, A., Vassar, M., MS, R., Vespa, P., Wang, K., Yue, J., Yuh, E., & Zafonte, R. (2021). Central Curation of Glasgow Outcome Scale-Extended Data: Lessons Learned from TRACK-TBI. Journal of Neurotrauma, 38 (17), 2419-2434. doi:10.1089/neu.2020.7528
Boehnlein, J., & Kinzie, J. (2021). Experiencing Mental Illness: Suffering, Hope, and Healing. Narrative Inquiry in Bioethics, 11 (2), 189-194. doi:10.1353/nib.2021.0070
Bohr, T., Hjorth, P., Holst, S., Hrabetová, S., Kiviniemi, V., Lilius, T., Lundgaard, I., Mardal, K., Martens, E., Mori, Y., Nägerl, U., Nicholson, C., Tannenbaum, A., Thomas, J., Tithof, J., Benveniste, H., Iliff, J. J., Kelley, D., & Nedergaard, M. (2022). The glymphatic system: Current understanding and modeling. iScience, 25 (9), 104987. doi:10.1016/j.isci.2022.104987
Brett, B., Gardner, R., Godbout, J., Dams-O’Connor, K., & Keene, C. (2022). Traumatic Brain Injury and Risk of Neurodegenerative Disorder. Biological Psychiatry, 91(5), 498-507. doi:10.1016/j.biopsych.2021.05.025
Burke, B., Latimer, C., Keene, C., Sonnen, J., McCormick, W., Bowen, J., McCurry, S., Larson, E., & Crane, P. (2021). Theoretical impact of the AT(N) framework on dementia using a community autopsy sample. Alzheimer's & Dementia, 17(12), 1879-1891. doi:10.1002/alz.12348
Burke, J., Gugger, J., Ding, K., Kim, J., Foreman, B., Yue, J., Puccio, A., Yuh, E., Sun, X., Rabinowitz, M., Vassar, M., Taylor, S., Winkler, E., Deng, H., McCrea, M., Stein, M., Robertson, C., Levin, H., Dikmen, S., Temkin, N., Barber, J., Giacino, J., Mukherjee, P., Wang, K., Okonkwo, D., Markowitz, A., Jain, S., Lowenstein, D., Manley, G., Diaz-Arrastia, R., Badjatia, N., Duhaime, A., Feeser, V., Gaudette, E., Gopinath, S., Keene, C., Korley, F., Madden, C., Merchant, R., Schnyer, D., & Zafonte, R. (2021). Association of Posttraumatic Epilepsy With 1-Year Outcomes After Traumatic Brain Injury. JAMA Network Open, 4 (12), e2140191. doi:10.1001/jamanetworkopen.2021.40191
Callaway, E., Dong, H., Ecker, J., Hawrylycz, M., Huang, Z., Lein, E., Ngai, J., Osten, P., Ren, B., Tolias, A., White, O., Zeng, H., Zhuang, X., Ascoli, G., Behrens, M., Chun, J., Feng, G., Gee, J., Ghosh, S., Halchenko, Y., Hertzano, R., Lim, B., Martone, M., Ng, L., Pachter, L., Ropelewski, A., Tickle, T., Yang, X., Zhang, K., Bakken, T., Berens, P., Daigle, T., Harris, J., Jorstad, N., Kalmbach, B., Kobak, D., Li, Y., Liu, H., Matho, K., Mukamel, E., Naeemi, M., Scala, F., Tan, P., Ting, J., Xie, F., Zhang, M., Zhang, Z., Zhou, J., Zingg, B., Armand, E., Yao, Z., Bertagnolli, D., Casper, T., Crichton, K., Dee, N., Diep, D., Ding, S., Dong, W., Dougherty, E., Fong, O., Goldman, M., Goldy, J., Hodge, R., Hu, L., Keene, C., Krienen, F., Kroll, M., Lake, B., Lathia, K., Linnarsson, S., Liu, C., Macosko, E., McCarroll, S., McMillen, D., Nadaf, N., Nguyen, T., Palmer, C., Pham, T., Plongthongkum, N., Reed, N., Regev, A., Rimorin, C., Romanow, W., Savoia, S., Siletti, K., Smith, K., Sulc, J., Tasic, B., Tieu, M., Torkelson, A., Tung, H., van Velthoven, C., Vanderburg, C., Yanny, A., Fang, R., Hou, X., Lucero, J., Osteen, J., Pinto-Duarte, A., Poirion, O., Preissl, S., Wang, X., Aldridge, A., Bartlett, A., Boggeman, L., O’Connor, C., Castanon, R., Chen, H., Fitzpatrick, C., Luo, C., Nery, J., Nunn, M., Rivkin, A., Tian, W., Dominguez, B., Ito-Cole, T., Jacobs, M., Jin, X., Lee, C., Lee, K., Miyazaki, P., Pang, Y., Rashid, M., Smith, J., Vu, M., Williams, E., Biancalani, T., Booeshaghi, A., Crow, M., Dudoit, S., Fischer, S., Gillis, J., Hu, Q., Kharchenko, P., Niu, S., Ntranos, V., Purdom, E., Risso, D., de Bézieux, H., Somasundaram, S., Street, K., Svensson, V., Vaishnav, E., Van den Berge, K., Welch, J., An, X., Bateup, H., Bowman, I., Chance, R., Foster, N., Galbavy, W., Gong, H., Gou, L., Hatfield, J., Hintiryan, H., Hirokawa, K., Kim, G., Kramer, D., Li, A., Li, X., Luo, Q., Muñoz-Castañeda, R., Stafford, D., Feng, Z., Jia, X., Jiang, S., Jiang, T., Kuang, X., Larsen, R., Lesnar, P., Li, Y., Li, Y., Liu, L., Peng, H., Qu, L., Ren, M., Ruan, Z., Shen, E., Song, Y., Wakeman, W., Wang, P., Wang, Y., Wang, Y., Yin, L., Yuan, J., Zhao, S., Zhao, X., Narasimhan, A., Palaniswamy, R., Banerjee, S., Ding, L., Huilgol, D., Huo, B., Kuo, H., Laturnus, S., Li, X., Mitra, P., Mizrachi, J., Wang, Q., Xie, P., Xiong, F., Yu, Y., Eichhorn, S., Berg, J., Bernabucci, M., Bernaerts, Y., Cadwell, C., Castro, J., Dalley, R., Hartmanis, L., Horwitz, G., Jiang, X., Ko, A., Miranda, E., Mulherkar, S., Nicovich, P., Owen, S., Sandberg, R., Sorensen, S., Tan, Z., Allen, S., Hockemeyer, D., Lee, A., Veldman, M., Adkins, R., Ament, S., Bravo, H., Carter, R., Chatterjee, A., Colantuoni, C., Crabtree, J., Creasy, H., Felix, V., Giglio, M., Herb, B., Kancherla, J., Mahurkar, A., McCracken, C., Nickel, L., Olley, D., Orvis, J., Schor, M., Hood, G., Dichter, B., Grauer, M., Helba, B., Bandrowski, A., Barkas, N., Carlin, B., D’Orazi, F., Degatano, K., Gillespie, T., Khajouei, F., Konwar, K., Thompson, C., Kelly, K., Mok, S., & Sunkin, S. (2021). A multimodal cell census and atlas of the mammalian primary motor cortex. Nature, 598 (7879), 86-102. doi:10.1038/s41586-021-03950-0
Campagnola, L., Seeman, S., Chartrand, T., Kim, L., Hoggarth, A., Gamlin, C., Ito, S., Trinh, J., Davoudian, P., Radaelli, C., Kim, M., Hage, T., Braun, T., Alfiler, L., Andrade, J., Bohn, P., Dalley, R., Henry, A., Kebede, S., Alice, M., Sandman, D., Williams, G., Larsen, R., Teeter, C., Daigle, T., Berry, K., Dotson, N., Enstrom, R., Gorham, M., Hupp, M., Dingman Lee, S., Ngo, K., Nicovich, P., Potekhina, L., Ransford, S., Gary, A., Goldy, J., McMillen, D., Pham, T., Tieu, M., Siverts, L., Walker, M., Farrell, C., Schroedter, M., Slaughterbeck, C., Cobb, C., Ellenbogen, R., Gwinn, R., Keene, C., Ko, A., Ojemann, J., Silbergeld, D., Carey, D., Casper, T., Crichton, K., Clark, M., Dee, N., Ellingwood, L., Gloe, J., Kroll, M., Sulc, J., Tung, H., Wadhwani, K., Brouner, K., Egdorf, T., Maxwell, M., McGraw, M., Pom, C., Ruiz, A., Bomben, J., Feng, D., Hejazinia, N., Shi, S., Szafer, A., Wakeman, W., Phillips, J., Bernard, A., Esposito, L., D’Orazi, F., Sunkin, S., Smith, K., Tasic, B., Arkhipov, A., Sorensen, S., Lein, E., Koch, C., Murphy, G., Zeng, H., & Jarsky, T. (2022). Local connectivity and synaptic dynamics in mouse and human neocortex. Science, 375, 6585. doi:10.1126/science.abj5861
Cheng, Z., Lozier, C. C., Lewis, M., O’Neil, M., Luoma, J. B., & Morasco, B. (2021). Investigating the role of psychological inflexibility, mindfulness, and self -compassion in PTSD. Journal of Contextual Behavioral Science, 22, 102-107.
Clouston, S., Hall, C., Kritikos, M., Bennett, D., DeKosky, S., Edwards, J., Finch, C., Kreisl, W., Mielke, M., Peskind, E. R., Raskind, M. A., Richards, M., Sloan, R., Spiro, A., Vasdev, N., Brackbill, R., Farfel, M., Horton, M., Lowe, S., Lucchini, R., Prezant, D., Reibman, J., Rosen, R., Seil, K., Zeig-Owens, R., Deri, Y., Diminich, E., Fausto, B., Gandy, S., Sano, M., Bromet, E., & Luft, B. (2022). Cognitive impairment and World Trade Centre-related exposures. Nature Reviews Neurology, 18 (2), 103-116. doi:10.1038/s41582-021-00576-8
Coffey, K. R., Lesiak, A., Marx, R., Vo, E., Garden, G., & Neumaier, J. F. (2022). A cAMP-Related Gene Network in Microglia Is Inversely Regulated by Morphine Tolerance and Withdrawal. Biological Psychiatry Global Open Science, 2(2), 180-189. doi:10.1016/j.bpsgos.2021.07.011
Coffey, K. R., Venkat, V., West, M. O., & Barker, D. J. (2021). Lateral preoptic area neurons signal cocaine self-administration behaviors. European Journal of Neuroscience, 54(7), 6397-6405.
Course, M., Gudsnuk, K., Keene, C., Bird, T., Jayadev, S., & Valdmanis, P. (2022). Aberrant splicing of PSEN2, but not PSEN1, in individuals with sporadic Alzheimer's disease. Brain. Advance online publication. doi:10.1093/brain/awac294
Damodarasamy, M., Khaing, Z., Hyde, J., Keene, C., Bentov, I., Banks, W., & Reed, M. (2022). Viable human brain microvessels for the study of aging and neurodegenerative diseases. Microvascular Research, 140, 104282. doi:10.1016/j.mvr.2021.104282
Dickstein, D., De Gasperi, R., Gama Sosa, M., Perez-Garcia, G., Short, J., Sosa, H., Perez, G., Tschiffely, A., Dams-O’Connor, K., Pullman, M., Knesaurek, K., Knutsen, A., Pham, D., Soleimani, L., Jordan, B., Gordon, W., Delman, B., Shumyatsky, G., Shahim, P., DeKosky, S., Stone, J., Peskind, E. R., Blennow, K., Zetterberg, H., Chance, S., Torso, M., Kostakoglu, L., Sano, M., Hof, P., Ahlers, S., Gandy, S., & Elder, G. (2021). Brain and blood biomarkers of tauopathy and neuronal injury in humans and rats with neurobehavioral syndromes following blast exposure. Molecular Psychiatry, 26 (10), 5940-5954. doi:10.1038/s41380-020-0674-z
Djerdjaj, A., Ng, A. J., Rieger, N. S., & Christianson, J. P. (2022). The basolateral amygdala to posterior insular cortex tract is necessary for social interaction with stressed juvenile rats. Behavioural brain research, 435, 114050. doi:10.1016/j.bbr.2022
Edelman, W., Kiianitsa, K., Virmani, T., Martinez, R., Young, J., Keene, C., Bird, T., Raskind, W., & Korvatska, O. (2022). Reduced gene dosage is a common mechanism of neuropathologies caused by ATP6AP2 splicing mutations. Parkinsonism & Related Disorders, 101, 31-38. doi:10.1016/j.parkreldis.2022.06.015
Eissman, J., Dumitrescu, L., Mahoney, E., Smith, A., Mukherjee, S., Lee, M., Scollard, P., Choi, S., Bush, W., Engelman, C., Lu, Q., Fardo, D., Trittschuh, E., Mez, J., Kaczorowski, C., Hernandez Saucedo, H., Widaman, K., Buckley, R., Properzi, M., Mormino, E., Yang, H., Harrison, T., Hedden, T., Nho, K., Andrews, S., Tommet, D., Hadad, N., Sanders, R., Ruderfer, D., Gifford, K., Zhong, X., Raghavan, N., Vardarajan, B., Pericak-Vance, M., Farrer, L., Wang, L., Cruchaga, C., Schellenberg, G., Cox, N., Haines, J., Keene, C., Saykin, A., Larson, E., Sperling, R., Mayeux, R., Cuccaro, M., Bennett, D., Schneider, J., Crane, P., Jefferson, A., & Hohman, T. (2022). Sex differences in the genetic architecture of cognitive resilience to Alzheimer’s disease. Brain, 145 (7), 2541-2554. doi:10.1093/brain/awac177
Elliott, J., McBride, A., Balba, N., Thomas, S., Pattinson, C., Morasco, B., Wilkerson, A., Gill, J., & Lim, M. (2022). Feasibility and preliminary efficacy for morning bright light therapy to improve sleep and plasma biomarkers in US Veterans with TBI. A prospective, open-label, single-arm trial. PLOS ONE, 17 (4), e0262955. doi:10.1371/journal.pone.0262955
Evans, K., Barton, R., Hendrickson, R. C., & LaPlante, L. (2022). Creating Safe Spaces for Those Who Have Lived through Intimate Partner Violence. Journal of Aggression, Maltreatment & Trauma, NA, 1-16. doi:10.1080/10926771.2022.2099774
Farrell, K., Iida, M., Cherry, J., Casella, A., Stein, T., Bieniek, K., Walker, J., Richardson, T., White, C., Alvarez, V., Huber, B., Dickson, D., Insausti, R., Dams-O'Connor, K., Vonsattel, J., Teich, A., Gearing, M., Glass, J., Troncoso, J., Frosch, M., Hyman, B., Murray, M., Attems, J., Flanagan, M., Mao, Q., Mesulam, M., Weintraub, S., Woltjer, R., Pham, T., Kofler, J., Schneider, J., Yu, L., Purohit, D., Haroutunian, V., Hof, P., Gandy, S., Sano, M., Beach, T., Poon, W., Kawas, C., Corrada, M., Rissman, R., Metcalf, J., Shuldberg, S., Salehi, B., Nelson, P., Trojanowski, J., Lee, E., Wolk, D., McMillan, C., Keene, C., Latimer, C., Montine, T., Kovacs, G., Lutz, M., Fischer, P., Perrin, R., Cairns, N., McKee, A., & Crary, J. (2022). Differential Vulnerability of Hippocampal Subfields in Primary Age-Related Tauopathy and Chronic Traumatic Encephalopathy. Journal of Neuropathology & Experimental Neurology. doi:10.1093/jnen/nlac066
Farrell, K., Kim, S., Han, N., Iida, M., Gonzalez, E., Otero-Garcia, M., Walker, J., Richardson, T., Renton, A., Andrews, S., Fulton-Howard, B., Humphrey, J., Vialle, R., Bowles, K., de Paiva Lopes, K., Whitney, K., Dangoor, D., Walsh, H., Marcora, E., Hefti, M., Casella, A., Sissoko, C., Kapoor, M., Novikova, G., Udine, E., Wong, G., Tang, W., Bhangale, T., Hunkapiller, J., Ayalon, G., Graham, R., Cherry, J., Cortes, E., Borukov, V., McKee, A., Stein, T., Vonsattel, J., Teich, A., Gearing, M., Glass, J., Troncoso, J., Frosch, M., Hyman, B., Dickson, D., Murray, M., Attems, J., Flanagan, M., Mao, Q., Mesulam, M., Weintraub, S., Woltjer, R., Pham, T., Kofler, J., Schneider, J., Yu, L., Purohit, D., Haroutunian, V., Hof, P., Gandy, S., Sano, M., Beach, T., Poon, W., Kawas, C., Corrada, M., Rissman, R., Metcalf, J., Shuldberg, S., Salehi, B., Nelson, P., Trojanowski, J., Lee, E., Wolk, D., McMillan, C., Keene, C., Latimer, C., Montine, T., Kovacs, G., Lutz, M., Fischer, P., Perrin, R., Cairns, N., Franklin, E., Cohen, H., Raj, T., Cobos, I., Frost, B., Goate, A., White III, C., & Crary, J. (2022). Genome-wide association study and functional validation implicates JADE1 in tauopathy. Acta Neuropathologica, 143 (1), 33-53. doi:10.1007/s00401-021-02379-z
Fathian, A., Jamali, Y., Raoufy, M., Weiner, M., Schuf, N., Rosen, H., Miller, B., Neylan, T., Hayes, J., Finley, S., Aisen, P., Khachaturian, Z., Thomas, R., Donohue, M., Walter, S., Gessert, D., Sather, T., Jiminez, G., Thal, L., Brewer, J., Vanderswag, H., Fleisher, A., Davis, M., Morrison, R., Petersen, R., Jack, C., Bernstein, M., Borowski, B., Gunter, J., Senjem, M., Vemuri, P., Jones, D., Kantarci, K., Ward, C., Mason, S., Albers, C., Knopman, D., Johnson, K., Jagust, W., Landau, S., Trojanowki, J., Shaw, L., Lee, V., Korecka, M., Figurski, M., Arnold, S., Karlawish, J., Wolk, D., Toga, A., Crawford, K., Neu, S., Schneider, L., Pawluczyk, S., Beccera, M., Teodoro, L., Spann, B., Beckett, L., Harvey, D., Fletcher, E., Carmichael, O., Olichney, J., DeCarli, C., Green, R., Sperling, R., Johnson, K., Marshall, G., Frey, M., Lane, B., Rosen, A., Tinklenberg, J., Saykin, A., Foroud, T., Shen, L., Faber, K., Kim, S., Nho, K., Farlow, M., Hake, A., Matthews, B., Herring, S., Hunt, C., Morris, J., Raichle, M., Holtzman, D., Cairns, N., Householder, E., Taylor-Reinwald, L., Ances, B., Carroll, M., Leon, S., Mintun, M., Schneider, S., Oliver, A., Raudin, L., Sorensen, G., Kuller, L., Mathis, C., Lopez, O., Oakley, M., Paul, S., Relkin, N., Chaing, G., Raudin, L., Davies, P., Fillit, H., Hefti, F., Mesulam, M., Kerwin, D., Mesulam, M., Lipowski, K., Wu, C., Johnson, N., Grafman, J., Potter, W., Snyder, P., Schwartz, A., Montine, T., Peskind, E. R., Fox, N., Thompson, P., Apostolova, L., Tingus, K., Woo, E., Silverman, D., Lu, P., Bartzokis, G., Koeppe, R., Heidebrink, J., Lord, J., Potkin, S., Preda, A., Nguyenv, D., Foster, N., Reiman, E., Chen, K., Fleisher, A., Tariot, P., Reeder, S., Potkin, S., Mulnard, R., Thai, G., Mc-Adams-Ortiz, C., Buckholtz, N., Hsiao, J., Albert, M., Albert, M., Onyike, C., D’Agostino, D., Kielb, S., Simpson, D., Frank, R., Kaye, J., Quinn, J., Lind, B., Carter, R., Dolen, S., Doody, R., Villanueva-Meyer, J., Chowdhury, M., Rountree, S., Dang, M., Stern, Y., Honig, L., Bell, K., Marson, D., Grifth, R., Clark, D., Geldmacher, D., Brockington, J., Roberson, E., Grossman, H., Mitsis, E., de Toledo-Morrell, L., Shah, R., Fleischman, D., Arfanakis, K., Duara, R., Varon, D., Greig, M., Roberts, P., Galvin, J., Cerbone, B., Michel, C., Rusinek, H., de Leon, M., Glodzik, L., De Santi, S., Doraiswamy, P., Petrella, J., Wong, T., James, O., Smith, C., Jicha, G., Hardy, P., Sinha, P., Oates, E., Conrad, G., Porsteinsson, A., Goldstein, B., Martin, K., Makino, K., Ismail, M., Brand, C., Womack, K., Mathews, D., Quiceno, M., Diaz-Arrastia, R., King, R., Weiner, M., Martin-Cook, K., DeVous, M., Levey, A., Lah, J., Cellar, J., Burns, J., Anderson, H., Swerdlow, R., Graf-Radford, N., Parftt, F., Kendall, T., Johnson, H., Dyck, C., Carson, R., MacAvoy, M., Chertkow, H., Bergman, H., Hosein, C., Black, S., Stefanovic, B., Caldwell, C., Hsiung, G., Feldman, H., Mudge, B., Assaly, M., Kertesz, A., Rogers, J., Bernick, C., Munic, D., Kertesz, A., Kertesz, A., Rogers, J., Finger, E., Pasternak, S., Rachinsky, I., Drost, D., Sadowsky, C., Martinez, W., Villena, T., Turner, R., Johnson, K., Reynolds, B., Sabbagh, M., Belden, C., Jacobson, S., Sirrel, S., Kowall, N., Killiany, R., Budson, A., Norbash, A., Johnson, P., Allard, J., Lerner, A., Ogrocki, P., Hudson, L., Kittur, S., Borrie, M., Lee, T., Bartha, R., Johnson, S., Asthana, S., Carlsson, C., Fruehling, J., Harding, S., Bates, V., Capote, H., Rainka, M., Scharre, D., Kataki, M., Adeli, A., Petrie, E. C., MD, Li, G., Zimmerman, E., Celmins, D., Brown, A., Pearlson, G., Blank, K., Anderson, K., Santulli, R., Kitzmiller, T., Schwartz, E., Sink, K., Williamson, J., Garg, P., Watkins, F., Ott, B., Querfurth, H., Tremont, G., Salloway, S., Malloy, P., & Correia, S. (2022). The trend of disruption in the functional brain network topology of Alzheimer’s disease. Scientific Reports, 12 (1), 14998. doi:10.1038/s41598-022-18987-y
Fontaine, H., Silva, P. R., Neiswanger, C., Tran, R., Abraham, A., Land, B., Neumaier, J. F., & Chavkin, C. (2022). Stress decreases serotonin tone in the nucleus accumbens in male mice to promote aversion and potentiate cocaine preference via decreased stimulation of 5-HT1B receptors. Neuropsychopharmacology, 47(4), 891-901. doi:10.1038/s41386-021-01178-0
Fraigne, J., Hendrickson, R. C., Raskind, M. A., & Peever, J. (2022). The role of catecholamines in sleep physiology and disease. In T. Kilduff & A. Krystal (Eds.), Principles and Practices of Sleep Medicine, 7th Edition (p. 000). Virtual: Elsevier.
Frye, B. M., Craft, S., Latimer, C. S., Keene, C. D., Montine, T. J., Register, T. C., Orr, M. E., Kavanagh, K., Macauley, S. L., & Shively, C. A. (2021). Aging-related Alzheimer's disease-like neuropathology and functional decline in captive vervet monkeys (Chlorocebus aethiops sabaeus). American journal of primatology, 83(11), e23260. doi:/10.1002/ajp.23260
Gaudette, É., Seabury, S., Temkin, N., Barber, J., DiGiorgio, A., Markowitz, A., Manley, G., Badjatia, N., Duhaime, A., Ferguson, A., Gopinath, S., Grandhi, R., Jha, R., Keene, C., Kitagawa, R., Mac Donald, C., Maddedn, C., McCrea, M., Mukherjee, P., Ngwenya, L., Okonkwo, D., Robertson, C., Rosenthal, E., Schneider, A., Schnyer, D., Stein, M., Taylor, S., Vassar, M., & Yue, J. (2022). Employment and Economic Outcomes of Participants With Mild Traumatic Brain Injury in the TRACK-TBI Study. JAMA Network Open, 5 (6), e2219444. doi:10.1001/jamanetworkopen.2022.19444
Hampel, H., Elhage, A., Shaw, L., Aisen, P., Chen, C., Lleó, A., Iwatsubo, T., Iwata, A., Yamada, M., Ikeuchi, T., Jia, J., Wang, H., Teunissen, C., Peskind, E. R., Blennow, K., Cummings, J., & Vergallo, A. (2022). The use of lumbar puncture and safety recommendations in Alzheimer's disease: a plain language summary. Neurodegenerative Disease Management, 12 (5), 221-229. doi:10.2217/nmt-2022-0012
Heath, L., Earls, J., Magis, A., Kornilov, S., Lovejoy, J., Funk, C., Rappaport, N., Logsdon, B., Mangravite, L., Kunkle, B., Martin, E., Naj, A., Ertekin-Taner, N., Golde, T., Hood, L., Price, N., Abner, E., Adams, P., Albert, M., Albin, R., Allen, M., Amlie-Wolf, A., Apostolova, L., Arnold, S., Asthana, S., Atwood, C., Baldwin, C., Barber, R., Barnes, L., Barral, S., Beach, T., Becker, J., Beecham, G., Beekly, D., Bennett, D., Bigio, E., Bird, T., Blacker, D., Boeve, B., Bowen, J., Boxer, A., Burke, J., Burns, J., Bush, W., Butkiewicz, M., Buxbaum, J., Cairns, N., Cantwell, L., Cao, C., Carlson, C., Carlsson, C., Carney, R., Chui, H., Crane, P., Cribbs, D., Crocco, E., Cuccaro, M., De Jager, P., DeCarli, C., Dick, M., Dickson, D., Dombroski, B., Doody, R., Duara, R., Ertekin-Taner, N., Evans, D., Faber, K., Fairchild, T., Fallon, K., Fardo, D., Farlow, M., Farrer, L., Ferris, S., Foroud, T., Frosch, M., Galasko, D., Gearing, M., Geschwind, D., Ghetti, B., Gilbert, J., Goate, A., Green, R., Growdon, J., Haines, J., Hakonarson, H., Hamilton, R., Hamilton-Nelson, K., Harrell, L., Honig, L., Huebinger, R., Huentelman, M., Hulette, C., Hyman, B., Jarvik, G., Jin, L., Jun, G., Kamboh, M., Karydas, A., Katz, M., Kaye, J., Keene, C., Kim, R., Kowall, N., Kramer, J., Kukull, W., Kunkle, B., Kuzma, A., LaFerla, F., Lah, J., Larson, E., Leverenz, J., Levey, A., Lieberman, A., Lipton, R., Lunetta, K., Lyketsos, C., Malamon, J., Marson, D., Martin, E., Martiniuk, F., Mash, D., Masliah, E., Mayeux, R., McCormick, W., McCurry, S., McDavid, A., McKee, A., Mesulam, M., Miller, B., Miller, C., Miller, J., Montine, T., Morris, J., Mukherjee, S., Myers, A., Naj, A., O’Bryant, S., Olichney, J., Parisi, J., Paulson, H., Pericak-Vance, M., Perry, W., Peskind, E. R., Petersen, R., Pierce, A., Poon, W., Potter, H., Qu, L., Quinn, J., Raj, A., Raskind, M. A., Reiman, E., Reisberg, B., Reisch, J., Reitz, C., Ringman, J., Roberson, E., Rogaeva, E., Rosen, H., Rosenberg, R., Royall, D., Sager, M., Sano, M., Saykin, A., Schellenberg, G., Schneider, J., Schneider, L., Seeley, W., Slifer, S., Smith, A., Song, Y., Sonnen, J., Spina, S., George-Hyslop, P., Stern, R., Swerdlow, R., Tang, M., Tanzi, R., Trojanowski, J., Troncoso, J., Tsuang, D., Valladares, O., Van Deerlin, V., Van Eldik, L., Vance, J., Vardarajan, B., Vinters, H., Vonsattel, J., Wang, L., Weintraub, S., Welsh-Bohmer, K., Whitehead, P., Wilhelmsen, K., Williamson, J., Wingo, T., Woltjer, R., Wright, C., Wu, C., Younkin, S., Yu, C., Yu, L., & Zhao, Y. (2022). Manifestations of Alzheimer’s disease genetic risk in the blood are evident in a multiomic analysis in healthy adults aged 18 to 90. Scientific Reports, 12 (1), 6117. doi:10.1038/s41598-022-09825-2
Hendrickson, R. C., Slevin, R., Hoerster, K., Chang, B., Sano, E., McCall, C., Monty, G., Thomas, R., & Raskind, M. A. (2022). The Impact of the COVID-19 Pandemic on Mental Health, Occupational Functioning, and Professional Retention Among Health Care Workers and First Responders. Journal of General Internal Medicine, 37 (2), 397-408. doi:10.1007/s11606-021-07252-z
Hubbard, E., Heil, L., Merrihew, G., Chhatwal, J., Farlow, M., McLean, C., Ghetti, B., Newell, K., Frosch, M., Bateman, R., Larson, E., Keene, C., Perrin, R., Montine, T., MacCoss, M., & Julian, R. (2022). Does Data-Independent Acquisition Data Contain Hidden Gems? A Case Study Related to Alzheimer’s Disease. Journal of Proteome Research, 21 (1), 118-131. doi:10.1021/acs.jproteome.1c00558
Hupfeld, K., Richmond, S., McGregor, H., Schwartz, D., Luther, M., Beltran, N., Kofman, I., De Dios, Y., Riascos, R., Wood, S., Bloomberg, J., Mulavara, A., Silbert, L., Iliff, J. J., Seidler, R., & Piantino, J. (2022). Longitudinal MRI-visible perivascular space (PVS) changes with long-duration spaceflight. Scientific Reports, 12 (1), 7238. doi:10.1038/s41598-022-11593-y
Hwangbo, N., Zhang, X., Raftery, D., Gu, H., Hu, S., Montine, T., Quinn, J., Chung, K., Hiller, A., Wang, D., Fei, Q., Bettcher, L., Zabetian, C., Peskind, E. R., Li, G., Promislow, D., & Franks, A. (2022). A Metabolomic Aging Clock Using Human Cerebrospinal Fluid. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 77(4), 744-754. doi:10.1093/gerona/glab212
Hwangbo, N., Zhang, X., Raftery, D., Gu, H., Hu, S., Montine, T., Quinn, J., Chung, K., Hiller, A., Wang, D., Fei, Q., Bettcher, L., Zabetian, C., Peskind, E. R., Li, G., Promislow, D., Davis, M., & Franks, A. (2022). Predictive Modeling of Alzheimer’s and Parkinson’s Disease Using Metabolomic and Lipidomic Profiles from Cerebrospinal Fluid. Metabolites, 12 (4), 277. doi:10.3390/metabo12040277
Iliff, J. J., & Penn, R. D. (2022). Extracellular Fluid Movement and Clearance in the Brain: The Glymphatic Pathway. In H. Richard Winn (Ed.), Yeoman’s Neurological Surgery, 8th Edition (p. 474). virtual: Elsevier.
Jacobs, D., Hitchcock, L., Williams, R. G., & Lattal, K. (2022). Effects of a cue associated with cocaine or food reinforcers on extinction and postextinction return of behavior. Behavioral Neuroscience, 136 (4), 307-317. doi:10.1037/bne0000519
Jansson, D., Wang, M., Thomas, R., Erickson, M., Peskind, E. R., Li, G., & Iliff, J. J. (2022). Markers of Cerebrovascular Injury, Inflammation, and Plasma Lipids Are Associated with Alzheimer’s Disease Cerebrospinal Fluid Biomarkers in Cognitively Normal Persons. Journal of Alzheimer's Disease, 86 (2), 813-826. doi:10.3233/JAD-215400
Jhanji, M., Rao, C., Massey, J., Hope, M., Zhou, X., Keene, C., Ma, T., Wyatt, M., Stewart, J., & Sajish, M. (2022). Cis- and trans-resveratrol have opposite effects on histone serine-ADP-ribosylation and tyrosine induced neurodegeneration. Nature Communications, 13 (1), 3244. doi:10.1038/s41467-022-30785-8
Katz, I., Rogers, M., Lew, R., Thwin, S., Doros, G., Ahearn, E., Ostacher, M., DeLisi, L., Smith, E., Ringer, R., Ferguson, R., Hoffman, B., Kaufman, J., Paik, J., Conrad, C., Holmberg, E., Boney, T., Huang, G., Liang, M., Agrawal, D., Akhtar, N., Androsenko, M., Berger, B., Bhat, V., Brenner, L., Chalasani, L., Chang, D., Chen, P., Cornejo, B., Cory, D., Davidson, D., Dickmann, P., Duncan, E., Fernando, R., Floyd, K., Forman, S., Gale, P., Geete, J., Ignatowski, M., Jones, K., Juergens, T., Jurjus, G., Khatkhate, G., Konicki, E., Krahn, D., Larson, G., Leckband, S., Mack, J., Matthews, S., Mayo, L., McGlade, E., Michalets, J., Miller, E., Muly, E., Niculescu, A., Ostacher, M., Padala, P., Padala, K., Pazzaglia, P., Raskind, M. A., Renshaw, P., Shivakumar, G., Smith, J., Sullivan, D., Suppes, P., Swann, A., Thomas, L., Thompson, S., Turner, E., Umbert, M., Westermeyer, J., Wood, A., Wortzel, H., & Yurgelun-Todd, D. (2022). Lithium Treatment in the Prevention of Repeat Suicide-Related Outcomes in Veterans With Major Depression or Bipolar Disorder. JAMA Psychiatry, 79 (1), 24. doi:10.1001/jamapsychiatry.2021.3170
Keil, S., Braun, M., O’Boyle, R., Sevao, M., Pedersen, T., Agarwal, S., Jansson, D., & Iliff, J. J. (2022). Dynamic infrared imaging of cerebrospinal fluid tracer influx into the brain. Neurophotonics, 9 (03), 031915. doi:10.1117/1.NPh.9.3.031915
Keil, S., Schindler, A., Wang, M., Lim, M., Piantino, J., Elliott, J., Werhane, M., Thomas, R., & Iliff, J. J. (2022). Longitudinal Sleep Instability Contributes to Cognitive Decline and Alzheimer's Pathology: Findings from the Seattle Longitudinal Study. SLEEP, 45 (Supplement 1), A283.
Latimer, C., Keene, C., Kraemer, B. C., & Liachko, N. F. (2021). TDP-43 promotes pathological tau phosphorylation and selective neurotoxicity in C. elegans. Alzheimer's and Dementia, 17 (S2), e058137. doi:10.1002/alz.058137
Latimer, C., Stair, J., Hincks, J., Currey, H., Bird, T., Keene, C., Kraemer, B., & Liachko, N. F. (2022). TDP-43 promotes tau accumulation and selective neurotoxicity in bigenic Caenorhabditis elegans. Disease Models and Mechanisms, 15 (4), dmm049323. doi:10.1242/dmm.049323
Lee, C., Latimer, C., Henriksen, J., Blazes, M., Larson, E., Crane, P., Keene, C., & Lee, A. (2021). Application of deep learning to understand resilience to Alzheimer's disease pathology. Brain Pathology, 31(6), e12974. doi:10.1111/bpa.12974
Lewis, M., Naugle, A. E., DiBacco, T. A., Katte, K., Smith, C. A., & Blematl, A. R. (2022). Behavioral measures of experiential avoidance: the role of context in predicting performance on two stressful tasks. Current Psychology, 41, 1-16. Retrieved from https://link.springer.com/article/10.1007/s12144-022-03447-7
Li, M., Kitamura, A., Beverley, J., Koudelka, J., Duncombe, J., Lennen, R., Jansen, M., Marshall, I., Platt, B., Wiegand, U., Carare, R., Kalaria, R., Iliff, J. J., & Horsburgh, K. (2022). Impaired Glymphatic Function and Pulsation Alterations in a Mouse Model of Vascular Cognitive Impairment. Frontiers in Aging Neuroscience, 13, 788519. doi:10.3389/fnagi.2021.788519
Li, Y. I., Rau, H., Engle, C. K., Gunn, H., Raskind, M. A., & Mayer, C. (2022). Characterizing actigraphy-measured sleep disturbances in Veterans with chronic post-traumatic headaches following mild traumatic brain injury. SLEEP, 45 (Supplement 1), A282.
Logsdon, A., Francis, K., Richardson, N., Hu, S., Faber, C., Phan, B., Nguyen, V., Setthavongsack, N., Banks, W., Woltjer, R., Keene, C., Latimer, C., Schwartz, M., Scarlett, J., & Alonge, K. (2022). Decoding perineuronal net glycan sulfation patterns in the Alzheimer's disease brain. Alzheimer's and Dementia, 18(5), 942-954. doi:10.1002/alz.12451
McDonagh, M., Morasco, B., Wagner, J., Ahmed, A., Fu, R., Kansagara, D., & Chou, R. (2022). Cannabis-Based Products for Chronic Pain. Annals of Internal Medicine, 175 (8), 1143-1153. doi:10.7326/m21-4520
McEvoy, C., Crabtree, A., Powell, J., Meabon, J., & Mihalik, J. (2022). Cumulative Blast Exposure Estimate Model for Special Operations Forces Combat Soldiers. Journal of Neurotrauma. Advance online publication. doi:10.1089/neu.2022.0075
Merlin, J., Althouse, A., Feldman, R., Arnsten, J., Bulls, H., Liebschutz, J., Nugent, S., Orris, S., Rohac, R., Starrels, J., Morasco, B., & Kansagara, D. (2021). Analysis of State Cannabis Laws and Dispensary Staff Recommendations to Adults Purchasing Medical Cannabis. JAMA Network Open, 4 (9), e2124511. doi:10.1001/jamanetworkopen.2021.24511
Nolan, A., Sohal, V., & Rosi, S. (2022). Selective Inhibitory Circuit Dysfunction after Chronic Frontal Lobe Contusion. The Journal of Neuroscience, 42 (27), 5361-5372. doi:10.1523/JNEUROSCI.0097-22.2022
Nugent, S., Lovejoy, T., Shull, S., Dobscha, S., & Morasco, B. (2021). Associations of Pain Numeric Rating Scale Scores Collected during Usual Care with Research Administered Patient Reported Pain Outcomes. Pain Medicine, 22 (10), 2235-2241. doi:10.1093/pm/pnab110
Nugent, S., Morasco, B., Handley, R., Clayburgh, D., Hooker, E., Ganzini, L., Knight, S., Chen, J., Sullivan, D., & Slatore, C. (2021). Risk of Suicidal Self-directed Violence Among US Veteran Survivors of Head and Neck Cancer. JAMA Otolaryngology–Head & Neck Surgery, 147 (11), 981. doi:10.1001/jamaoto.2021.2625
O’Neil, M., Klyce, D. W., Pogoda, T. K., Cifu, D. X., Eggleston, B. E., Cameron, D. C., Wilde, E. A., Walker, W. C., & Carlson, K. F. (2021). Associations among PTSD and postconcussive symptoms in the long-term impact of military-relevant brain injury consortium-chronic effects of neurotrauma consortium prospective, longitudinal study. Journal of Head Trauma Rehabilitation, 36(6), E363-E372. doi: 10.1097/HTR.0000000000000665
Otero, M., Rau, H., Shofer, J., Peskind, E. R., & Pagulayan, K. F. (2022). Self-perceived irritability among OEF/OIF/OND veterans with a history of deployment-related mTBI: Associations with prospective memory and quality of life. The Clinical Neuropsychologist, 36 (6), 1384-1404. doi:10.1080/13854046.2020.1856413
Pease, M., Arefan, D., Barber, J., Yuh, E., Puccio, A., Hochberger, K., Nwachuku, E., Roy, S., Casillo, S., Temkin, N., Okonkwo, D., Wu, S., Badjatia, N., Bodien, Y., Duhaime, A., Feeser, V., Ferguson, A., Foreman, B., Gardner, R., Gopinath, S., Keene, C., Madden, C., McCrea, M., Mukherjee, P., Ngwenya, L., Schnyer, D., Taylor, S., & Yue, J. (2022). Outcome Prediction in Patients with Severe Traumatic Brain Injury Using Deep Learning from Head CT Scans. Radiology, 12(1), 6117. doi:10.1148/radiol.212181
Pedersen, T., Keil, S., Agarwal, S., Badran, M., Gozal, D., & Iliff, J. J. (2022). Impact of Chronic Sleep Disruption on Glymphatic Function, Cognitive Performance, and Neuropathology in the FXFAD Mouse Model. SLEEP, 45 (Supplement 1), A126.
Phongpreecha, T., Gajera, C., Liu, C., Vijayaragavan, K., Chang, A., Becker, M., Fallahzadeh, R., Fernandez, R., Postupna, N., Sherfield, E., Tebaykin, D., Latimer, C., Shively, C., Register, T., Craft, S., Montine, K., Fox, E., Poston, K., Keene, C., Angelo, M., Bendall, S., Aghaeepour, N., & Montine, T. (2021). Single-synapse analyses of Alzheimer’s disease implicate pathologic tau, DJ1, CD47, and ApoE. Science Advances, 7 (51), eabk0473. doi:10.1126/sciadv.abk0473
Piantino, J., Iliff, J. J., & Lim, M. (2022). The Bidirectional Link Between Sleep Disturbances and Traumatic Brain Injury Symptoms: A Role for Glymphatic Dysfunction?. Biological Psychiatry, 91(5), 478-487. doi:10.1016/j.biopsych.2021.06.025
Prater, K., Green, K., Chiou, K., Smith, C., Sun, W., Shojaie, A., Heath, L., Rose, S., Keene, C., Logsdon, B., Snyder-Mackler, N., Blue, E., Young, J., Garden, G., & Jayadev, S. (2021). Microglia subtype transcriptomes differ between Alzheimer Disease and control human postmortem brain samples. Alzheimer's and Dementia, 17 (S2), e058474. doi:10.1002/alz.058474
Ray, L., Pike, M., Simon, M., Iliff, J. J., & Heys, J. (2021). Quantitative analysis of macroscopic solute transport in the murine brain. Fluids and Barriers of the CNS, 18 (1), 55. doi:10.1186/s12987-021-00290-z
Rieger, N. S., Guoynes, C. D., Monari, P. K., Hammond, E. R., Malone, C. L., & Marler, C. A. (2022). Neuroendocrine mechanisms of aggression in rodents. Motivation Science, 8(2), 81-105. Retrieved from https://doi.org/10.1037/mot0000260
Rieger, N. S., Varela, J. A., Ng, A. J., Granata, L., Djerdjaj, A., Brenhouse, H. C., & Christianson, J. P. (2022). Insular cortex corticotropin-releasing factor integrates stress signaling with social affective behavior. Neuropsychopharmacology, 47(6), 1156-1168. doi:10.1038/s41386-022-01292-7
Rieger, N. S., Worley, N., Ng, A., & Christianson, J. (2022). Insular cortex modulates social avoidance of sick rats. Behavioural Brain Research, 416, 113541. doi:10.1016/j.bbr.2021.113541
Salman, M., Kitchen, P., Halsey, A., Wang, M., Törnroth-Horsefield, S., Conner, A., Badaut, J., Iliff, J. J., & Bill, R. (2022). Emerging roles for dynamic aquaporin-4 subcellular relocalization in CNS water homeostasis. Brain, 145 (1), 64-75. doi:10.1093/brain/awab311
Schindler, A. G., Baskin, B., Juarez, B., Janet Lee, S., Hendrickson, R., Pagulayan, K., Zweifel, L. S., Raskind, M. A., Phillips, P. E. M., Peskind, E. R., & Cook, D. G. (2021). Repetitive blast mild traumatic brain injury increases ethanol sensitivity in male mice and risky drinking behavior in male combat veterans. Alcoholism, clinical and experimental research, 45(5), 1051–1064. doi:10.1111/acer.14605
Schneider, L., Bennett, D., Farlow, M., Peskind, E. R., Raskind, M. A., Sano, M., Stern, Y., Haneline, S., Welsh-Bohmer, K., O’Neil, J., Walter, R., Maresca, S., Culp, M., Alexander, R., Saunders, A., Burns, D., & Chiang, C. (2022). Adjudicating Mild Cognitive Impairment Due to Alzheimer’s Disease as a Novel Endpoint Event in the TOMMORROW Prevention Clinical Trial. The Journal of Prevention of Alzheimer's Disease, 9(4), 625-634. doi:10.14283/jpad.2022.72
Sheppard, D., Rau, H., Trittschuh, E., Werhane, M., Schindler, A., Hendrickson, R. C., Peskind, E. R., & Pagulayan, K. F. (2022). Poorer prospective memory performance is associated with reduced time monitoring among OEF/OIF/OND Veterans with a history of blast-related mild traumatic brain injury. The Clinical Neuropsychologist. doi:10.1080/13854046.2022.2068455
Sheppard, D., Rau, H., Werhane, M., Fonseca, L., Chaytor, N., Peskind, E. R., & Pagulayan, K. F. (2022). Associations between Intra-Individual Neurocognitive Variability and Prospective Memory in Veterans with Mild Traumatic Brain Injury History and Posttraumatic Stress Disorder. Archives of Clinical Neuropsychology, 37(6), 1221-1227. doi:10.1093/arclin/acac014
Simon, M., Wang, M., Ismail, O., Braun, M., Schindler, A., Reemmer, J., Wang, Z., Haveliwala, M., O’Boyle, R., Han, W., Roese, N., Grafe, M., Woltjer, R., Boison, D., & Iliff, J. J. (2022). Loss of perivascular aquaporin-4 localization impairs glymphatic exchange and promotes amyloid ß plaque formation in mice. Alzheimer's Research and Therapy, 14 (1), 59. doi:10.1186/s13195-022-00999-5
Somohano, V., Kaplan, J., Newman, A., O’Neil, M., & Lovejoy, T. (2022). Formal mindfulness practice predicts reductions in PTSD symptom severity following a mindfulness-based intervention for women with co-occurring PTSD and substance use disorder. Addiction Science & Clinical Practice, 17 (1), 51. doi:10.1186/s13722-022-00333-2
Somohano, V., Shank, T., Manuel, J., Mallik, D., Rehder, K., & Bowen, S. (2021). The Role of Pretreatment Expectancy on Substance Use Outcomes in Women Mandated to Mindfulness-Based Relapse Prevention. The Journal of Alternative and Complementary Medicine. doi:10.1089/acm.2021.0123
Sorg, S., Werhane, M., Merritt, V., Clark, A., Holiday, K., Hanson, K., Jak, A. J., Schiehser, D. M., & Delano-Wood, L. (2021). Research letter: PTSD symptom severity and multiple traumatic brain injuries are associated with elevated memory complaints in veterans with histories of mild TBI. Journal of Head Trauma Rehabilitation, 36 (6), 418-423. doi:10.1097/HTR.0000000000000659
Sun, D., Rakesh, G., Clarke-Rubright, E., Haswell, C., Logue, M. W., O’Leary, E., Cotton, A., Xie, H., Dennis, E., Jahanshad, N., Salminen, L., Thomopoulos, S., Rashid, F., Ching, C., Koch, S., Frijling, J., Nawijn, L., van Zuiden, M., Zhu, X., Suarez-Jimenez, B., Sierk, A., Walter, H., Manthey, A., Stevens, J., Fani, N., van Rooij, S., Stein, M., Bomyea, J., Koerte, I., Choi, K., van de Werff, S., Vermeiren, R., Herzog, J., Lebois, L., Baker, J., Ressler, K., Olson, E., Straube, T., Korgaonkar, M., Andrew, E., Zhu, Y., Li, G., Ipser, J., Hudson, A., Peverill, M., Sambrook, K., Gordon, E., Baugh, L., Forster, G., Simons, R., Simons, J., Magnotta, V., Maron-Katz, A., du Plessis, S., Disner, S., Davenport, N., Grupe, D., Nitschke, J., deRoon-Cassini, T., Fitzgerald, J., Krystal, J. H., Levy, I., Olff, M., Veltman, D., Wang, L., Neria, Y., De Bellis, M., Jovanovic, T., Daniels, J., Shenton, M., van de Wee, N., Schmahl, C., Kaufman, M., Rosso, I., Sponheim, S., Hofmann, D., Bryant, R., Fercho, K., Stein, D., Mueller, S., Phan, L., McLaughlin, K., Davidson, R., Larson, C., May, G., Nelson, S., Abdallah, C., Gomaa, H., Etkin, A., Seedat, S., Harpaz-Rotem, I., Liberzon, I., Wang, X., Thompson, P., & Morey, R. (2022). Remodeling of the cortical structural connectome in posttraumatic stress disorder: Results from the ENIGMA-PGC PTSD consortium. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. Advance online publication. doi:10.1016/j.bpsc.2022.02.008
Sytsma, T., Chen, D., Rolf, B., Dorschner, M., Jayadev, S., Keene, C., Zhang, J., Bird, T., & Latimer, C. (2022). Spinal cord-predominant neuropathology in an adult-onset case of POLR3A-related spastic ataxia. Neuropathology, 42 (1), 58-65. doi:10.1111/neup.12775
Tian, C., Stewart, T., Hong, Z., Guo, Z., Aro, P., Soltys, D., Pan, C., Peskind, E. R., Zabetian, C., Shaw, L., Galasko, D., Quinn, J., Shi, M., & Zhang, J. (2022). Blood extracellular vesicles carrying synaptic function- and brain-related proteins as potential biomarkers for Alzheimer's disease. Alzheimer's & Dementia. doi:10.1002/alz.12723
Torres, E., Luo, J., Boehnlein, J., Towns, D., Kinzie, J., DeBarber, A., & Raber, J. (2022). Apolipoprotein E Isoform-specific changes related to stress and trauma exposure. Translational Psychiatry, 12 (1), 125-135. doi:10.1038/s41398-022-01848-7
Uneri, A., Niere, F., Macauley, S., Ma, T., Keene, C., Craft, S., & Raab-Graham, K. (2021). mRNA-Binding Protein DJ-1 as a pivotal protein in AD pathology. Alzheimer's and Dementia, 17 (S2), e058602. doi:10.1002/alz.058602
Williams, R. G., Li, K., & Phillips, P. (2022). The Influence of Stress on Decision-Making: Effects of CRF and Dopamine Antagonism in the Nucleus Accumbens. Frontiers in Psychiatry, 12, 113541. doi:10.3389/fpsyt.2021.814218
Wyse, J., Mackey, K., Lovejoy, T., Kansagara, D., Tuepker, A., Gordon, A., Todd Korthuis, P., Herreid-O’Neill, A., Williams, B., & Morasco, B. (2022). Expanding access to medications for opioid use disorder through locally-initiated implementation. Addiction Science & Clinical Practice, 17 (1), 32. doi:10.1186/s13722-022-00312-7
Wyse, J., Morasco, B., Dougherty, J., Edwards, B., Kansagara, D., Gordon, A., Korthuis, P., Tuepker, A., Lindner, S., Mackey, K., Williams, B., Herreid-O’Neill, A., Paynter, R., & Lovejoy, T. (2021). Adjunct interventions to standard medical management of buprenorphine in outpatient settings: A systematic review of the evidence. Drug and Alcohol Dependence, 228, 108923. doi:10.1016/j.drugalcdep.2021.108923
Sign up for email updates or access your subscriber preferences: https://public.govdelivery.com/accounts/USVHAVISN20/subscriber/new.
Use of these Materials and Finding VA Health Care
Please note that the health care information provided in these materials is for educational purposes only. It does not replace the role of a medical practitioner for advice on care and treatment. If you are looking for professional medical care, find your local VA healthcare center by using the VA Facilities Locator & Directory. This page may contain links that will take you outside of the Department of Veterans Affairs website. VA does not endorse and is not responsible for the content of the linked websites.
VA Web Disclaimers
Disclaimer of Endorsement: Reference herein to any specific commercial products, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government, and shall not be used for advertising or product endorsement purposes.
Disclaimer of Hyperlinks: The appearance of external hyperlinks does not constitute endorsement by the Department of Veterans Affairs of the linked websites, or the information, products or services contained therein. For other than authorized VA activities, the Department does not exercise any editorial control over the information you may find at these locations. All links are provided with the intent of meeting the mission of the Department and the VA website. Please let us know about existing external links which you believe are inappropriate and about specific additional external links which you believe ought to be included.
Disclaimer of Liability: With respect to documents available from this server, neither the United States Government nor any of its employees, makes any warranty, express or implied, including the warranties of merchantability and fitness for a particular purpose, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights.
Reference from this web page or from any of the information services sponsored by the VA to any non-governmental entity, product, service or information does not constitute an endorsement or recommendation by the VA or any of its employees. We are not responsible for the content of any "off-site" web pages referenced from this server.
Disclaimer: The sharing of any non-VA information does not constitute an endorsement of products or services on the part of the VA.
![]()
VA Regional Offices
 The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
Find out if you can get VA health care as a Veteran
The following four categories of Veterans are not required to enroll but are urged to do so to permit better planning of health resources:
- Veterans with a service-connected (SC) disability rated at 50% or more.
- Veterans seeking care for a disability the military determined was incurred or aggravated in the line of duty, but which VA has not yet rated, within 12 months of discharge.
- Veterans seeking care for a SC disability only or under a special treatment authority.
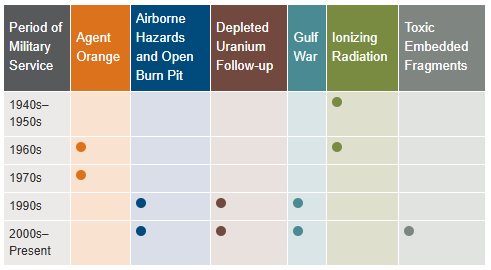
- Veterans seeking health registry examinations. VA’s health registry evaluation is a free, voluntary medical assessment for Veterans who may have been exposed to certain environmental hazards during military service. The evaluations alert Veterans to possible long-term health problems that may be related to exposure to specific environmental hazards during their military service. VA has established several health registries to track and monitor the health of specific groups of Veterans. You may be eligible to participate in one or more of these health registries: Agent Orange Registry, Airborne Hazards and Open Burn Pit Registry, Gulf War Registry (includes Operations Iraqi Freedom and New Dawn), Ionizing Radiation Registry, Depleted Uranium Follow-Up Program, and Toxic Embedded Fragment Surveillance Center. Use the chart below to help determine your eligibility.
Find out how to apply for VA health care benefits as a Veteran or service member. For other mental health services, contact a VA medical center for information on eligibility and treatment options.
Community Care (Mission Act)
The MISSION Act became law in 2018, bringing the VA’s previous Veterans Choice Program to an end and establishing the Community Care Program. VA provides health care for Veterans from providers in your local community outside of VA. Veterans may be eligible to receive care from a community provider when VA cannot provide the care needed. This care is provided on behalf of and paid for by VA. Community care is also available to Veterans based on certain conditions and eligibility requirements, and in consideration of a Veteran’s specific needs and circumstances. VA offers urgent care services to eligible Veterans at in-network urgent care clinics to treat minor injuries and illnesses that are not life-threatening, such as colds, strep throat, sprained muscles, and skin and ear infections. Community care must be first authorized by VA before a Veteran can receive care from a community provider.
Vet Centers in VISN 20
 Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Alaska
| Anchorage Vet Center (Anchorage, AK) | Fairbanks Vet Center (Fairbanks, AK) |
| Kenai Vet Center Outstation (Soldotna, AK) | Wasilla Vet Center (Wasilla, AK) |
Idaho
| Boise Vet Center (Boise, ID) | East Idaho Vet Center (Idaho Falls, ID) |
Oregon
| Central Oregon Vet Center (Bend, OR) | Eugene Vet Center (Eugene, OR) |
| Grants Pass Vet Center (Grants Pass, OR) | Portland, OR Vet Center (Portland, OR) |
| Salem Vet Center (Salem, OR) |
Washington
Plan your trip to VA
 In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
VCS operates over 200 Patriot Stores in Veterans Administration (VA) Medical Centers nationwide. Many of our stores have been recently updated and expanded to provide our customers with a modern, clean and comfortable shopping experience. Our stores welcome our customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations.
The Patriot Cafe is the best place in the VA Medical Center to enjoy delicious, freshly prepared breakfast or lunch served hot or cold each weekday. Providing Veterans, their families, VA employees, volunteers and visitors a place to relax and enjoy a meal or take-out for their convenience. With a wide variety of food from traditional comfort food, specialized menu selections and a large assortment of healthy choices; there is something for everyone's taste buds.
Hospital Service Directory
To find out whether there is a van near you use the Disabled American Veterans (DAV) Hospital Service Coordinator Directory to contact your nearest HSC for information or assistance. Please remember that the DAV Transportation Network is staffed by volunteers; therefore, it is unable to cover every community. The vans are driven by volunteers, and the rides coordinated by more than 133 Hospital Service Coordinators around the country. Our nation’s heroes travel around the globe to protect our freedoms—it’s only right that we return their dedication. Volunteering to drive a Vet ensures that even those living remotely from VA hospitals can make their appointments and never go without the treatment they need. Learn more about the DAV transportation network through the VISN 20 NewsFlash Resources section.
 Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
VA Puget Sound Health Care System (VAPSHCS) serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. Veterans Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA Outpatient Clinics and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
VA Portland Health Care System (VAPORHCS) serves Veterans in Oregon and Southwest Washington with two main divisions: Portland VA Medical Center and Vancouver VA Medical Center. Veterans Medical Centers are also located in Roseburg, White City, and Vancouver, Washington. VA Outpatient Clinics and Vet Centers are located in Astoria, Bend, Boardman, Brookings, Eugene, Fairview, Grants Pass, Hines, Hillsboro, Klamath Falls, LaGrande, Lincoln City, Newport, Portland, Salem, The Dalles, and West Linn.