Intensive Case Management
PSCI-SPC Intensive Case Management
Case management focuses on building a collaborative relationship between the therapist and the client to facilitate assessment, evaluation, care coordination, and advocacy on behalf of the client and addresses individual needs (Case Management Society of America, 2017). Intensive case management, or ICM, assists in coordination of care, which increases access. Additionally, ICM provides resources addressing social determinants of health and allows the case manager to provide streamlined and enhanced care to meet the Veteran's needs. Therefore, Transit and SUPERCEDE's version of ICM involves the assigning a case manager who ensures the Veteran establishes a continuity of holistic care and health care needs by connecting them to providers and services both within VA and in VA community care.
Transit - community organizations
A brief psychosocial intervention for Veterans who are at risk for suicide and ineligible for or disengaged from VA careTransit was a Transitional Care Program pilot that provided Veterans at risk for suicide and not eligible or engaged in VA healthcare services with brief psychotherapy and intensive case management services to address any pressing acute mental health needs and to support their connection to VA or community providers. The intervention concurrently supported at-risk Veterans' acute needs and their transition to more comprehensive VA or community-based resources, depending on their VA eligibility status. Veterans enrolled in TRANSIT received immediate and short-term psychotherapy to provide symptom relief, intensive case management and follow-up, a crisis response plan, as well as referrals to community mental health placement by the TRANSIT suicide prevention coordinator.
Supercede - VA/community care
Suicide Prevention intensive Case management and coordination in community care 2.0 - SUPERCEDE - This program tested the feasibility of a suicide prevention intensive case management (ICM) intervention to increase access to high quality mental health services for Veterans who are at risk for suicide. This intervention combined a modular version of Brief Cognitive Behavioral Therapy for Suicide Prevention (Bryan & Rudd, 2018) with intensive case management, and coordination of VA care and VA authorized community care. This intervention aimed to ensure Veterans at risk for suicide who were referred out to the community for physical health care services received timely access to specialty mental health care. This intervention focused on providing Veterans at-risk for suicide or who experienced severe mental health symptoms and experience psychosocial needs with resources to address risk factors known to contribute to suicidal ideation, such as unemployment or housing resources. Veterans enrolled in SUPERCEDE received immediate and short-term psychotherapy to provide symptom relief, intensive case management and follow-up, a crisis response plan, as well as referrals to community mental health placement by the SUPERCEDE suicide prevention coordinator.
Note: The VA SRM Superceed Manual is currently down for extended maintenance while we improve the accessibility. Thanks for your patience and we apologize for the inconvenience.
The VA SRM Superceed Manual will be here when it is available
Supercede-RCT - VA/community care
SUPERCEDE-RCT is a hybrid type 2 clinical trial further examining the feasibility and acceptability of SUPERCEDE.
The next steps of the SUPERCEDE intervention are to conduct a Randomized Controlled trial of the intervention. The trial will be conducted in 100 Veterans. SUPERCEDE will be compared to the current standard of VA care. This project is underway.
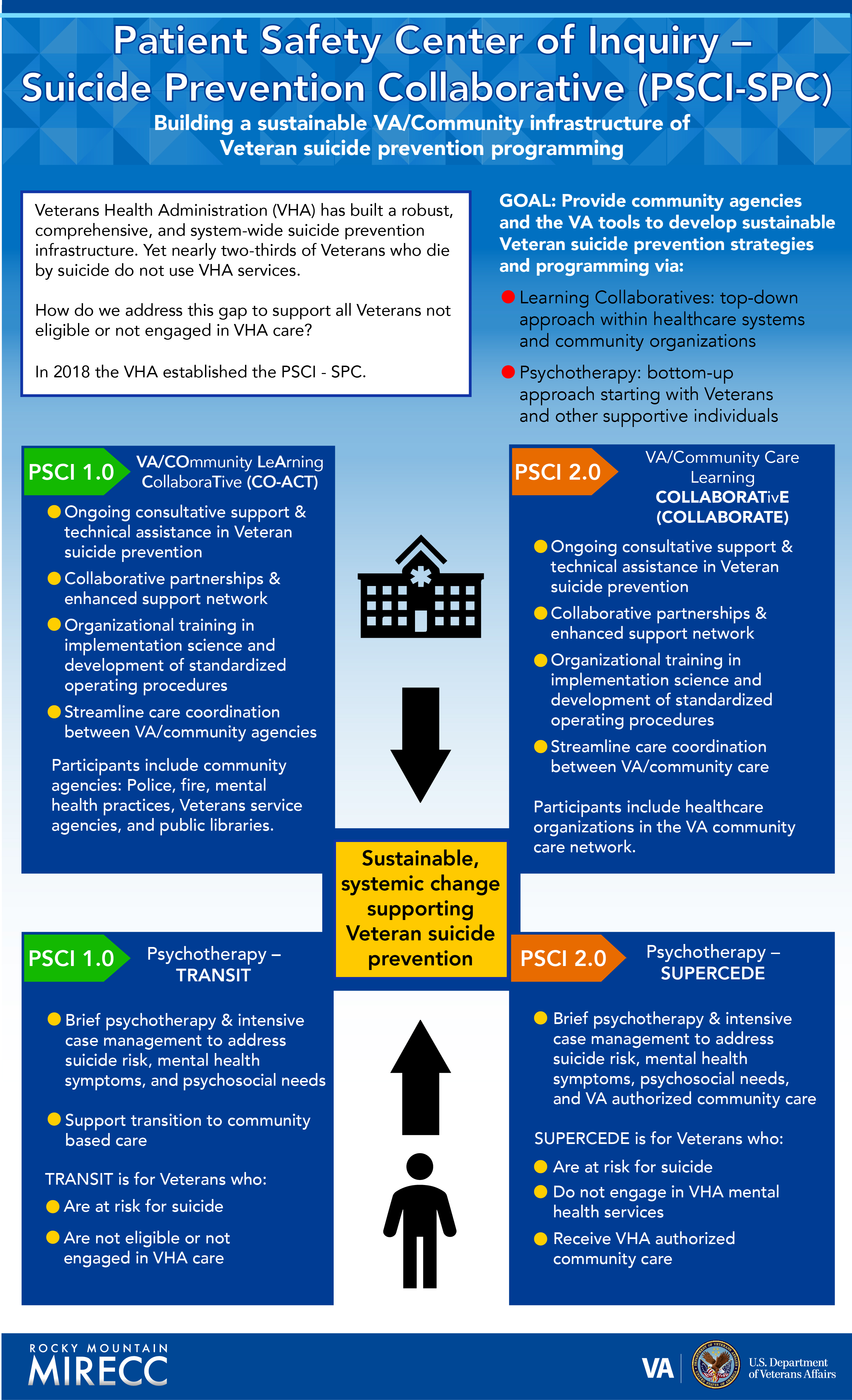
Patient Safety Center of Inquiry - Suicide Prevention Collaborative (PSCI-SPC)
Building a sustainable VA/Community infrastructure of Veteran suicide preventiori programming
Veterans Health Administration (VHA) has built a robust, comprehensive, and system-wide suicide prevention infrastructure. Yet nearly two-thirds of Veterans who die by suicide do not use VHA services.
How do we address this gap to support all Veterans not eligible or not engaged in VHA care?
In 2018 the VHA established the PSCI - SPC.
GOAL: Provide community agencies and the VA tools to develop sustainable Veteran suicide prevention strategies and programming via:
- Learning Collaboratives: top-down approach within healthcare systems and community organizations
- Psychotherapy: bottom-up approach starting with Veterans and other supportive individuals
Sustainable, systemic change supporting Veteran suicide prevention
PSCI 1.0
VA/Community Learning Collaborative (CO-ACT)
- Ongoing consultative support & technical assistance in Veteran suicide prevention
- Collaborative partnerships & enhanced support network
- Organizational training in implementation science and develpment of standardized operating procedures
- Streamline care coordination between VA/community agencies
Participants iinclude community agencies: Police, fire, mental health practices, Veterans services agencies, and public libaries.
Psychotherapy - TRANSIT
- Brief psychotherapy & intensive case management to address sucide risk, mental health symptoms, and psychosocial needs
- Support transition to community based care
TRANSIT is for Veterans who:
- Are at risk for sucide
- Are not eligible or not engaged in VHA care
PSCI 2.0
VA/Community Care Learning COLLABORATIVE (COLLABORATE)
- Ongoing consultative support & technical assistance in Veteran sucide prevention
- Collaborative partnerships & enhanced support network
- Organizational training in implementation science and development of standardized operatiing procedures
- Streamline care coordination between VA/community care
Participants include healthcare organization in the VA community care network.
Psychotherapy - SUPERCEDE
- Brief psychotherapy & intensive case management to address sucude risk, mental health symptoms, psychosocial needs, and VA authorized community care
SUPERCEDE is for Veterans who:
- Are at risk for suicide
- Do not engage in VHA mental health services
- Recieve VHA authorized community care



















