Collaborative Care

Dynamic Diffusion
Learning Collaborative
This video is intended for use by VA staff who wish to introduce Veterans and/or other staff to moral injury groups. The Veterans in this video are real people who participated in a moral injury group facilitated by a psychiatrist and a chaplain in Nashville, TN. The group focused on male Veterans with combat-related moral injury, though moral injury encompasses a diverse array of experiences and can affect any Veteran. For more information, visit the VA Diffusion Marketplace website.
What is the Dynamic Diffusion Network?
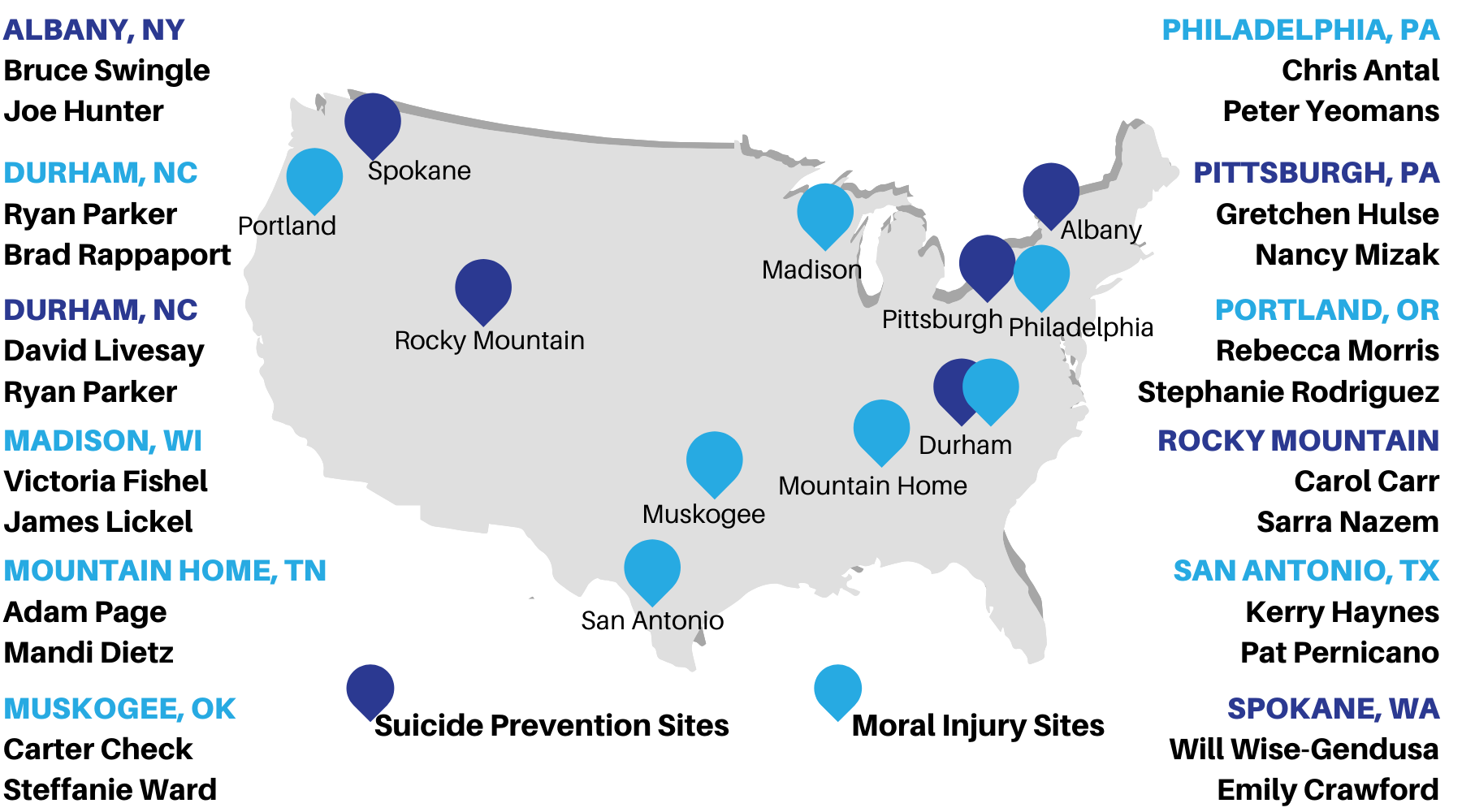
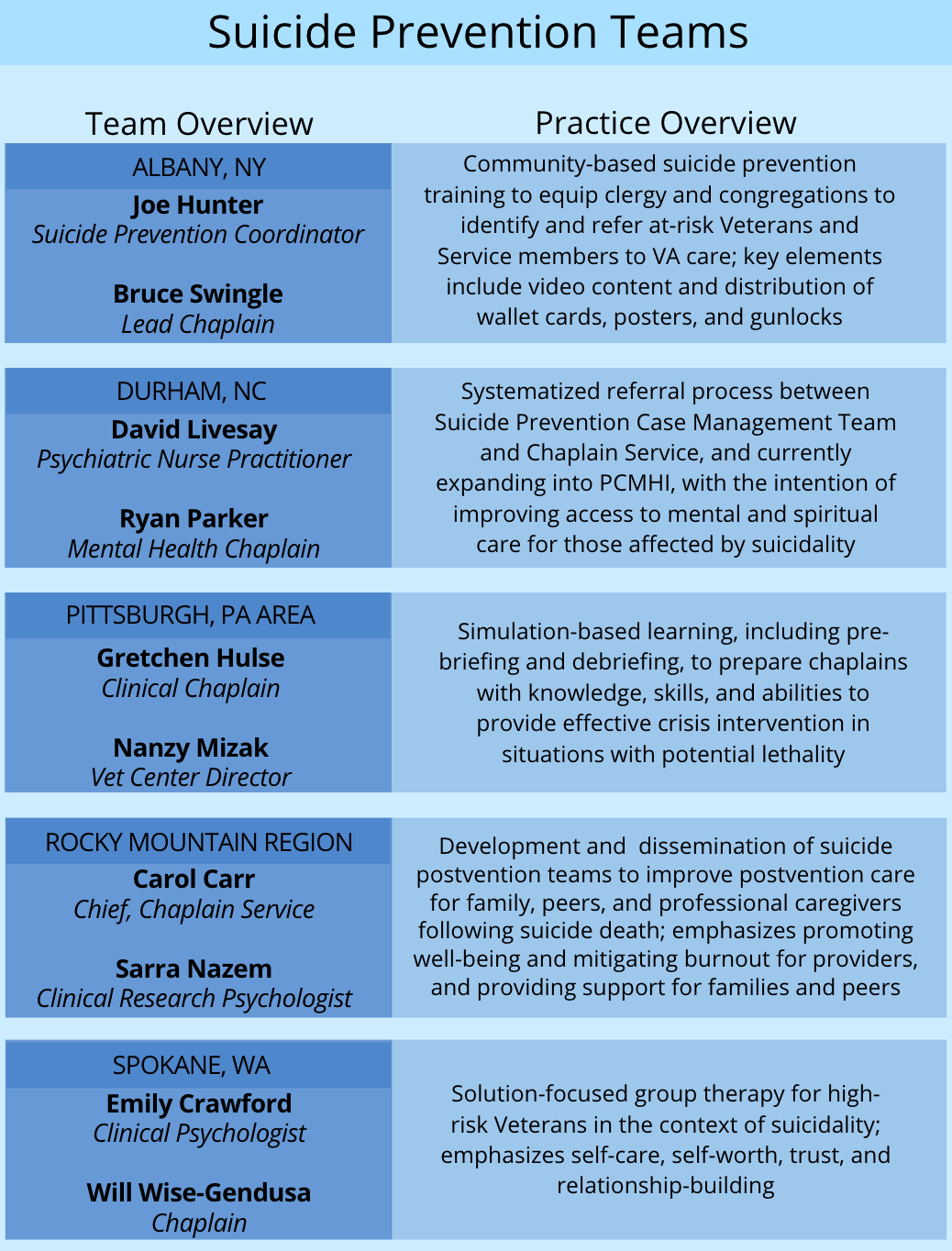
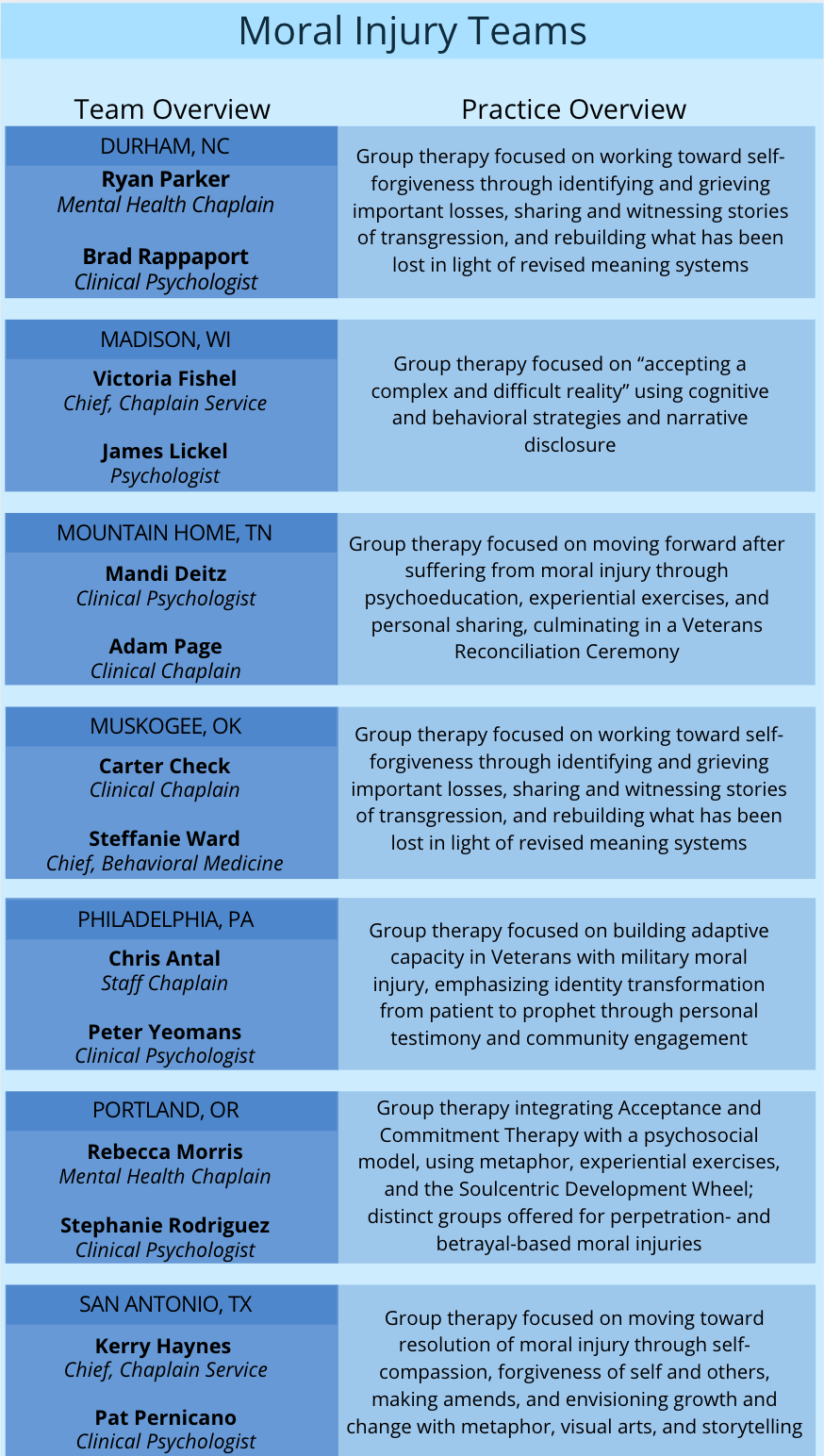
A network of IMH-trained chaplains* and mental health partners who have been identified as leaders in the areas of suicide prevention and moral injury based on approaches they have developed to address these complex problems.
What is “dynamic diffusion”?
An innovative approach to development and dissemination. Care practices are delivered and continuously evaluated under real-world conditions as part of a structured network experience that promotes cross-pollination of ideas and shared learning to generate relatively rapid improvements in care.
*Integrative Mental Health offers a recurring, intensive Mental Health Integration for Chaplain Services (MHICS) training. Chaplains in the Dynamic Diffusion Network have completed MHICS and/or the IMH Learning Collaborative (see tab above).
Participating Sites
Practice Descriptions
For more information about these practices, contact Integrative Mental Health at IMH@va.gov
Building on recommendations from the VA/DoD Integrated Mental Health Strategy, VA and DoD conducted a "learning collaborative" that brought together teams from 14 medical centers across the country to focus on better integrating mental health and chaplain services at their respective sites. Teams utilized the learning collaborative methodology to employ systems redesign principles to improve their clinical care. In the case of Mental Health and Chaplaincy Learning Collaborative, this entailed improving: mutual awareness between mental health and chaplaincy; practices for communicating and coordinating care; and formalized methods for integration. The three videos below describe the learning collaborative rationale, process, and findings; highlighting practical experiences from successful participating teams.
Videos
Model for Integration |
| Teams were guided by the below model to help them focus on better integrating care across six domains: screening and referrals (i.e., patient flow practices); communication, documentation, and assessment (i.e., professional practices); and role clarification and cross-disciplinary training (i.e., interdisciplinary relationships). Teams came together on three separate occasions over the course of a year to focus on different points of the model (first patient flow, then professional practices, then interdisciplinary relationships), sharing system improvement approaches and metrics with one another along the way. |
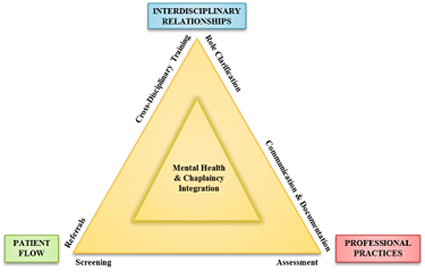
Specifically, the six aims of the learning collaborative are to strengthen and improve: |
||||||||||||||||
|
||||||||||||||||
The overall objectives of the learning collaborative were to: |
||||||||||||||||
|
||||||||||||||||
The Integrative Mental Health Program partnered with the Defense Centers of Excellence, the VA Center for Applied Systems Engineering (VA-CASE), and the Durham Health Services Research and Development Center of Innovation (HSR&D) to conduct this learning collaborative. Participating sites are listed below.
|