TBI 101
Traumatic Brain Injury (TBI) is a common but complicated form of injury. The impact of TBI on an individual's health and functioning varies widely.
What factors determine the course of illness and subsequent recovery?
- Severity of injury (i.e., mild, moderate or severe)
- Comorbid neuropsychiatric and medical conditions (e.g., depression, substance use disorders, chronic pain, sleep disturbances, PTSD)
- Psychosocial circumstances (e.g., connectedness and/or loneliness, finances, access to care)
If an injury is not properly identified, or physical and/or mental sequelae are not adequately addressed, this may contribute to lingering or unresolved symptoms.
Clinical presentations and TBI-related courses of illness can be quite diverse. Clinicians should focus on other pertinent neuropsychiatric and psychosocial factors in addition to the original neuronal injury. The following content provides introductory information about TBI, its management, common definitions, criteria pertaining to injury severity, epidemiology and sequelae.
 Defining TBI
Defining TBI
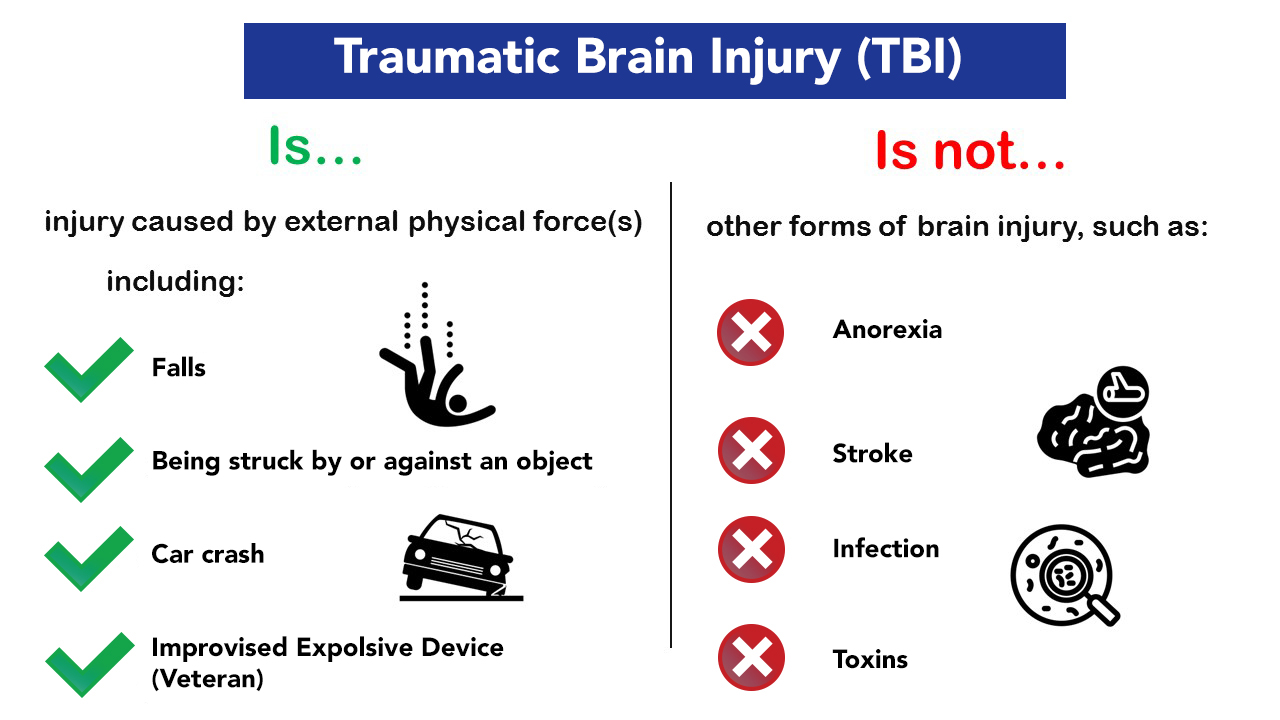
Traumatic Brain Injury (TBI) is defined as a disruption in brain function and/or structure caused by the application of external physical forces (e.g., acceleration/deceleration, blast) that produce an acute (i.e., immediate) disruption of cognitive and/or elementary neurological functions. 1, 2, 3, 4 In more simple terms, forces acting on the brain render a person unconscious, dazed, or confused at the time of injury. The term TBI should be strictly reserved for injuries caused by external physical forces and is not applicable to other forms of brain injury (e.g., anoxia, stroke, infection, toxins).
Cause of Injury and Severity
Penetrating, or open-head, TBIs involve an object that breaches the skull and invades brain tissue, such as a bullet or piece of shrapnel. Outcomes from penetrating injuries are dictated by the nature and extent of neuroanatomy damaged by the penetrating object(s), and frequently involve additional medical complications, such as bleeding and infection.
Non-penetrating, or closed-head, TBIs represent the vast majority of TBIs and refer to those injuries in which the cranium remains intact. Non-penetrating injuries are much more common, and are typically rated in severity as either mild, moderate, or severe.
The prognosis for a TBI is usually informed by injury severity. Although there are several approaches for assessing TBI severity, the most widely accepted criteria is offered by the American Congress of Rehabilitation Medicine (ACRM). 4
The ACRM criteria for mild, moderate, and severe TBI are echoed both in the DSM-5 and the VA/DoD Clinical Practice Guidelines (CPGs) for Management and Rehabilitation of Post-Acute Mild Traumatic Brain Injury (mTBI)
Classification of TBI Severity
| (If a patient meets criteria in more than one category of severity, the higher severity level is assigned.) | |||
|---|---|---|---|
| Criteria | Mild | Moderate | Severe |
| Structural imaging | Normal | Normal or abnormal | Normal or abnormal |
| Loss of consciousness/metal state (LOC) | 0-30 min | > 30 min and < 24 hours | > 24 hours |
| Alteration of consciousness/mental state (AOC)* | Up to 24 hours | > 24 hours; severity based on other criteria | > 24 hours; severity based on other criteria |
| Posttraumatic amnesia (PTA) | 0-1 day | > 1 and < 7 days | > 7 days |
| Glasgow Coma Scale (GCS) (best available score in first 24 hours)** | 13-15 | 9-12 | < 9 |
| * Alteration of mental status must be immediately related to the trauma to the head. Typical symptoms would be looking and feeling dazed and uncertain of what is happening, confusion, and difficulty thinking clearly or responding appropriately to mental status questions, and being unable to describe events immediately before or after the trauma event. | |||
| ** In April 2015, the DoD released a memorandum recommending against the use of GCS scores to diagnose TBI. See the memorandum for additional information. 3 | |||
 Epidemiology
Epidemiology
The CDC reports 64,362 TBI related deaths in 2020, representing 176 deaths per day. 220,000 TBI related hospitalizations occurred in 2019, representing over 611 hospitalizations per day.
Surveillance data indicates nearly 2.5 million TBI-related emergency department visits per year.
Seventy percent of TBI-related emergency room visits are the consequence of the three leading mechanisms of injury:
- falls
- being struck by or against an object
- motor vehicle crashes
The most common mechanism of injury for those aged 15-24 and 25-34 was motor vehicle crashes. Data suggests that most injuries, nearly 80%, are mild in severity. 5
Some age-related differences include an increase in emergency room visits secondary to sports and/or recreation related TBIs sustained by children (under the age of 19) which grew by 57% over the preceding decade. Data suggests that a similar increase in older adult falls (resulting from a growing aging population) may also be a partial driver in an upward trend of TBIs. In fact, falls remain a leading cause of TBI at both ends of the age spectrum. 5
However, these numbers are likely an underrepresentation. Mild TBIs often go untreated and thus are not detected in settings where surveillance efforts are implemented, such as the emergency department, urgent care, or primary care. These factors make it difficult to precisely determine the frequency of such injuries.
It is important to be aware of unique risks factors and TBI-related challenges for specific populations as certain groups and communities have markedly different rates of TBI as noted in our TBI & Special Populations Section below.
TBI Sequelae & Prognosis
Though there is considerable variability across individuals and outcomes, the natural history of TBI is well-established and there remain some predictable aspects of recovery regarding the course and resolution of symptoms.
It is important that patients and clinicians keep in mind that the terms mild, moderate, and severe refer to parameters surrounding the acute injury event (i.e., duration of unconsciousness, duration of posttraumatic amnesia, GCS scores), and do not denote outcomes.
Across all severities of TBI, symptoms and impairment tend to be most severe and demonstrable immediately following injury. Thereafter, gradual improvement is the typical trajectory of illness, with the speed and extent of recovery largely influenced by the initial level of severity. Late-emerging symptoms and/or downward trajectories are unusual following TBI, often suggesting the need to consider alternative explanations (other than the initial TBI itself). 6
Moderate-Severe TBI
Moderate-Severe TBI features a broad spectrum of potential outcomes, relative to mild TBI, ranging from death or devastating neuropsychiatric impairment to remarkable recovery that may even approximate the individual's pre-injury baseline status.
Mild TBI
Mild TBI involves a much narrower spectrum of outcomes related to the direct effects of neurotrauma. The natural history and prognosis for a single mild TBI is well-established in the medical literature, involving a very favorable long-term prognosis in most cases. 7 Mild TBI was consistently associated with cognitive deficits in the first 48 hours to two weeks following injury, but recovery frequently occurred early thereafter (during the first month after injury). Limited evidence exists to support the idea that complete recovery may take longer (up to six months or a year for some), or that long-standing severe neurocognitive impairment was present following a concussion.
A subset of individuals do remain who experience persisting symptoms following TBI.
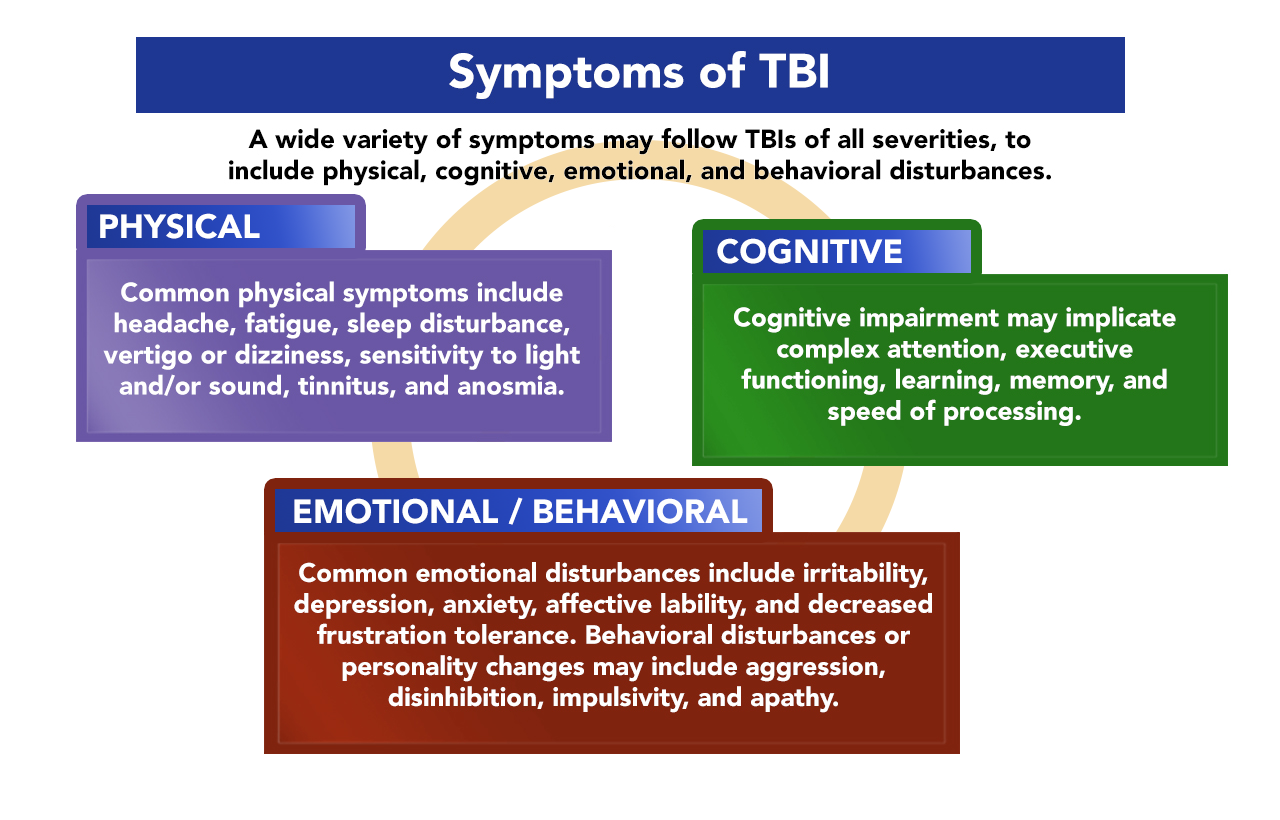
A wide variety of symptoms may follow TBIs of all severities, to include physical, cognitive, emotional, and behavioral disturbances. Common physical symptoms include headache, fatigue, sleep disturbance, vertigo or dizziness, sensitivity to light and/or sound, tinnitus, and anosmia. Cognitive impairment may implicate complex attention, executive functioning, learning, memory, and speed of processing. Common emotional disturbances include irritability, depression, anxiety, affective lability, and decreased frustration tolerance. Behavioral disturbances or personality changes may include aggression, disinhibition, impulsivity, and apathy.
Such atypical recovery occurs in about 10% of cases, and these outcomes are largely influenced by non "brain injury" related factors. Comprehensive evaluation and management of TBI necessitates a comprehensive approach to all the medical, psychological, and psychosocial circumstances which may influence an individual's course of illness following TBI.
 Post TBI Physical Impact
Post TBI Physical Impact
It is not uncommon for those who sustain a TBI to also experience a physical condition secondary to the injury. Bowel and bladder incontinence, hemiparesis, comorbid spinal cord injury, and medical complications arising from increased risk of certain conditions in the first year after a TBI can introduce setbacks during one's recovery journey. Such impairments may feel as though they greatly hinder progress toward recovery. However, these concerns are typically addressed during post-acute rehabilitation and are incorporated into treatment goals to allow for a successful transition back to one's community.
Additional physical impairments may persist after one's discharge from an inpatient or outpatient therapy program, or in the chronic phase of brain injury recovery, considered as being six months or greater post-TBI. 8 Such long-term impairments may include:
- cognitive function
- chronic pain
- vision impairment
- chronic fatigue
In this section of the TBI toolkit, you will find an overview of these four concerns, plus information regarding their prevalence among TBI survivors.
TBI & Cognitive Function
Cognitive processes that may be impacted by TBI include:
- attention
- information processing
- memory
- planning and executing tasks
- decision-making
- recognition of appropriate social cues 9, 10, 11
Visit Model Systems Knowledge Translation center "Cognition Problems after Traumatic Brain Injury" page for more information and helpful strategies.
The prevalence of cognitive deficits varies across the phases of TBI recovery and injury severity level. 12 The prevalence from acute to subacute phases of injury decreases over time for mild TBI. In contrast, moderate-severe TBI cases show a greater occurrence of impacted attention, information processing speed, and memory into the chronic phase of recovery. Impact on cognition is often one of the "invisible" effects of TBI that can impact relationships, ability to hold stable employment, and motivation to keep up with activities of daily living. 13, 14
Chronic impairment to cognitive processes have been associated with continued risk of cognitive decline as an individual ages. Individuals with a history of TBI may be at a higher risk for cognitive conditions commonly seen in older adults (e.g., Alzheimer's) when compared to those without TBI.
Please visit our Interventions page for recommendations and treatment strategies.TBI & Pain
Pain affects TBI survivors in various ways, but long-term strategies exist for many to manage pain levels throughout typical activities of daily life.
Chronic pain may arise from:
- injuries sustained with the TBI, such as bone fractures;
- physical conditions that arise because of the TBI, such as muscle spasticity, joint subluxation, gout, and neuropathic pain;
- and conditions resulting from the impact of the injury itself, such as headaches at the site of impact or migraines from light sensitivity
There is no one-size-fits-all approach when it comes to addressing chronic TBI-related pain, as there are many potentially significant factors that may contribute to one individual's pain. 15 Over half of individuals with TBI experience chronic pain, regardless of TBI severity, although a greater injury severity is correlated with increased likelihood of pain reported after injury. 16
The mechanisms from which pain results (e.g., neuroinflammation, axonal degeneration, and excitotoxicity) have been well studied; however, the extent to which individual patients are affected by these mechanisms is unknown. 17 For an in-depth review of chronic pain after TBI, review the study, Characterization and Treatment of Chronic Pain after Moderate to Severe Traumatic Brain Injury, by the Traumatic Brain Injury Model Systems National Data and Statistical Center.
Please visit our Interventions page for recommendations and treatment strategies.TBI, Vestibular & Vision
The vestibular system, located in the inner ear, involves processing sensory and visual information during activities of daily living.
According to the Brain Injury Association of America, up to 50% of TBI survivors experience vestibular impairments. 18 When these processes are disrupted, as is common in TBI, the individual may experience:
- hearing loss such as tinnitus
- balance and mobility problems
- visual problems (double vision, depth perception, and apraxia or ataxia) 19
For a further review of vestibular concerns after TBI, see the Brain Injury Guidelines webpage, which provides information about specific treatment tools used for vision and vestibular rehabilitation.
Please visit our Interventions page for recommendations and treatment strategies.TBI, Fatigue & Sleep Disorders
TBI-related fatigue commonly occurs secondary to mental and physical overexertion when completing highly complex tasks that require significant concentration, effort, or stamina. Fatigue may also appear as psychological fatigue, which can impede restful sleep and affect many aspects of mental as well as physical health. Insomnia and other sleep related issues are one of the most widely reported concerns by TBI survivors. Some sleep disturbances an individual may face after a brain injury include:
- excessive daytime sleepiness;
- difficulty falling or staying asleep;
- sleep apnea;
- insomnia;
- and hypersomnia
Level of injury severity may impact the prevalence of sleep related concerns, as they are identified in nearly half of those patients with moderate to severe TBIs. 20 Sleep disturbances may appear at any phase of brain injury recovery, thereby exacerbating cognitive concerns. 21 If a patient begins to experience sleep disturbances in the chronic phase of recovery, it is important to discuss treatment options with a health care provider. Sleep is vital in making continual progress towards recovery.
Sleep concerns can often be managed in the following ways:
- medication management (e.g., melatonin, pain management);
- sleep hygiene techniques (e.g., monitoring screen time during evening ours);
- light therapy
- limiting caffeine intake
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
A fact sheet with more information on fatigue and brain injury is available for download here at the Model Systems Knowledge Translation Center webpage. 22
Please visit our Interventions page for recommendations and treatment strategies. Post TBI Mental Health Impact
Post TBI Mental Health Impact
Co-occurring mental health issues and psychosocial difficulties are often some of the most disabling consequences of TBI and greatly impact the socio-economic aspects of health care costs. 23, 24 Pre-existing psychiatric conditions can be further exacerbated post-injury and may present as undesirable behavior that is maladaptive in recovery, e.g., increased irritability, emotional or physical outbursts, personality changes, and more. 25, 26
While there are many co-occurring mental health concerns that can impact individuals with a history of TBI, the following section will focus on the most common:
- substance misuse/
abuse - depression
- post-traumatic stress disorder (PTSD)
- suicide risk
To learn about the effects of community relationships and person-centered care on the mental health outcomes of persons with TBI, review this special issue of Brain Impairment by the Cambridge University Press. 27
TBI & Substance Use
Problems with substance use may occur in response to stress or in combination with other mental health and medical conditions. Pre-injury substance abuse not only increases the risk for sustaining a TBI, but also increases the risk of worsening recovery outcomes, and subsequent future TBIs. 28
As reported in Brain Injury Medicine, alcohol is the most misused substance after TBI (estimated 37% to 66%), compared to illicit drug abuse (between 10% and 44%). 29 It has been suggested that there is no safe amount of alcohol consumption after a brain injury, as it may impact the brain's natural healing process and could even cause further damage. It is essential for providers to routinely assess substance use in the ongoing management of individuals who sustained a TBI.
To learn more about how substance abuse impacts TBI recovery, review the webpage BrainLine for information regarding risk factors for post-injury substance misuse and treatment approaches. 30 The Ohio Valley Center for Brain Injury Prevention and Rehabilitation also provides useful information about working with individuals with TBI and substance use disorders.
Please visit our Interventions page for recommendations and treatment strategies.TBI & Depression
Individuals who have sustained a TBI face a risk, three times higher, for developing depression than the general population (Hellewell et al., 2020). The risk of depression after a TBI increases, regardless of injury severity, and can fluctuate over time if left untreated (Hart et al., 2012). As one of the most common psychiatric concerns to emerge after a TBI, it is imperative that depressive mood is addressed early on in the rehabilitation journey, as long-term mismanagement of symptoms may result in further cognitive decline and physical complications. Depression represents one of the most common psychiatric concerns that emerges after a TBI. If it is not addressed early in the rehabilitation journey, long-term symptom mismanagement may result in further cognitive decline and physical complications. Early identification and treatment of depression improves many outcomes.
Multiple factors contribute to the causes of depression following a TBI, including:
- Physical changes to areas of the brain that control emotions, or changes in the level of neurotransmitters
- Emotional response to injury due to adjustment issues and role changes
- Pre-existing factors unrelated to the injury, such as personal or family history
- Changes in functioning and level of independence that challenge identify and self-management
- Self-regulation may also be affected post-injury, resulting in greater difficulty for the individual and caregivers in managing emotions
If a patient experiences feelings of worthlessness, hopelessness, and sadness, it may be beneficial to discuss these feelings with a healthcare provider. They can recommend treatments specific to an individual's needs, such as medication or therapy, that may aid in getting back to a healthy and happy life. To learn more about depression symptoms and options for treatment, visit the Brain Injury Association of America for online resources.
Please visit our Interventions page for recommendations and treatment strategies.TBI & PTSD
It is not uncommon for brain injuries sustained in traumatic situations to result in the development of Post-Traumatic Stress Disorder (PTSD), with trauma severity correlating with risk of developing PTSD. Individuals with mild TBI were found to be 2.8 times more likely to develop a psychiatric disorder like PTSD than individuals with no history of TBI. 31
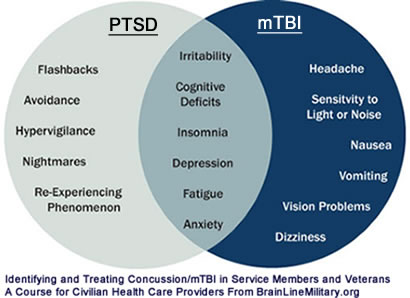
Many people who develop PTSD get better. Yet it remains important to monitor symptoms and triggers throughout one's life, and to check in with a healthcare provider regarding an increase of symptom severity. TBI symptoms typically tend to decrease within three to six months after the injury, whereas PTSD symptoms may last much longer, in turn potentially requiring continued therapy to address prolonged symptoms. 32 Separating symptoms of TBI and Post Traumatic Stress Disorder (PTSD) is a challenging process. The diagram below shows a sample of some common symptoms of PTSD and mild TBI.
The Health.mil webpage provides information and tips for civilian providers regarding treating military members with TBI and PTSD. The National Center for PTSD offers many resources for individuals and caregivers, including a self-screening tool for PTSD that can be used to determine if symptoms warrant a follow-up discussion with a healthcare provided.
Please visit our Interventions page for recommendations and treatment strategies.TBI & Suicide Risk
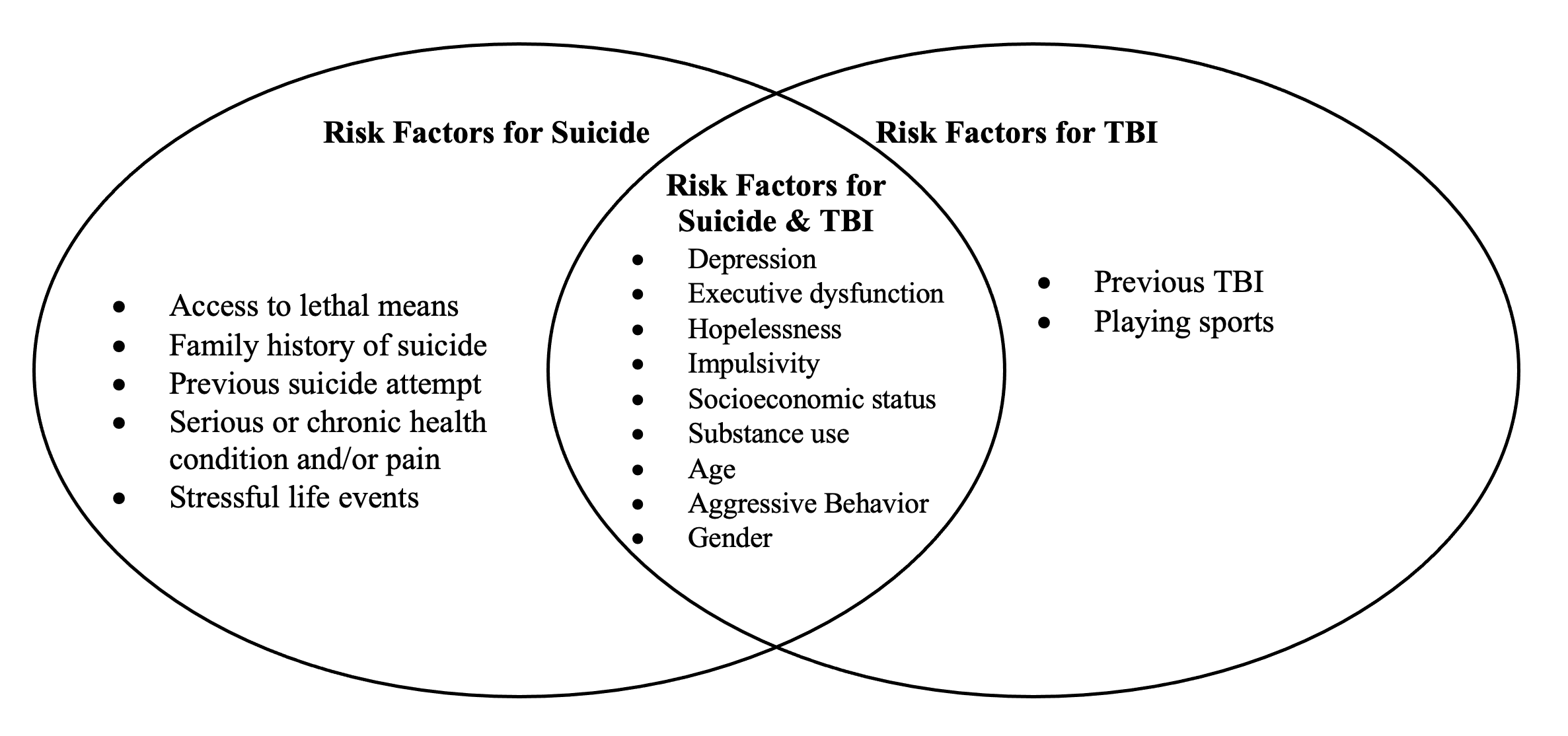
Traumatic brain injury poses significant mental health challenges for survivors, one of the greatest risks being suicidal ideation and suicide attempts. In a study conducted with Veterans seeking government health services, the risk for suicide was 2.19 times higher in Veterans with TBI compared to those without TBI. Veterans with moderate to severe TBI were also at an increased risk of death by lethal means such as firearms, as opposed to death by suicide using less lethal means in civilians without TBI. 33 When compared to the general population, individuals with TBI are three to four times more likely to die by suicide. 34
Considering that the TBI population is at a greater risk for suicide than the general population, it is important to consider what factors may exist in one's life that contribute to suicide risk, such as:
Comorbid health diagnoses and socio-economic concerns collectively impact the overall well-being of individuals with TBI. These risk factors may introduce obstacles to continued recovery in the chronic phase.
To learn more about suicide risk and prevention best practices review the VA/DOD Clinical Practice Guidelines for Suicide Prevention. Individuals struggling with thoughts of suicide should consult with a mental health provider regarding options for therapy and medication management. Individuals needing support or experiencing a suicidal crisis can contact the Suicide & Crisis Lifeline by dialing 988; Press 1 for the Veterans Crisis Line. There is also an online chat option for the Veterans Crisis Line.
Please visit our Interventions page for recommendations and treatment strategies. TBI & Special Populations
TBI & Special Populations
For best outcomes, providers should always aim to offer a person-centered approach to care. This requires consideration of an individual's unique constellation of neuropsychiatric, neurophysiological, physical, emotional, and cognitive changes following TBI. However, it is also important to be aware of unique risks factors and TBI-related challenges for specific populations. As described below, certain groups and communities have markedly different rates of TBI, resulting in health disparities that will impact life-long health trajectories post-injury. Reducing such disparities is an essential part of TBI prevention efforts as and helps reduce the likelihood of TBI resulting in chronic health conditions.
TBI & Military/Veterans: Introduction
TBI is an important issue facing military service members and Veterans. Increased risk for TBI in this population is likely due to several factors such as exposure to combat events (e.g., blasts, hard parachute landings), and training exercises (e.g., ropes courses, physical combat training). Other behaviors that are not job-related (e.g., vehicular crashes, risky behaviors, sports) may also increase risk
TBI & Military/Veterans: Background
Between 2000 and 2021, more than 450,000 U.S. Service members were diagnosed with a TBI. Several earlier conflicts during this period (OEF, OIF, OND, GWT) were associated with a dramatic increase in the prevalence of TBI due to blast injuries. Blast-related TBI injuries are those that are caused by the rapid transmission of acoustic waves through brain tissue as a result from close exposure to an explosion, such as those resulting from IEDs, mortars and landmines. TBI and mTBI related to blast injuries came to be called the "signature injury" of the OEF/OIF/OND conflict era. Most of these blast injuries were classified as mild. 36 Yet concern among researchers and medical professionals grew as persistent patterns of cognitive and behavioral change continued to be observed in service members and Veterans, despite little physical evidence of lasting damage to brain structures.
Research in this area provides evidence that mTBI, including those resulting from blast injuries, particularly multiple blast injuries, can result in post-concussive syndrome (PCS). In addition, service members and Veterans are at risk for other non-brain injury related conditions that may exacerbate the effects of TBI such as PTSD. 35 This is especially problematic because of the resulting exponential risk for significant symptoms that overlap between the two conditions: irritability, fatigue, anxiety, poor concentration, disturbed sleep and depressive symptoms. 36, 37 These symptoms may further complicate recovery by presenting significant challenges to maintaining service in the military and/or transitioning to civilian life after separating from service.
Please visit our Interventions page for recommendations and treatment strategies.TBI & Justice Involved: Introduction
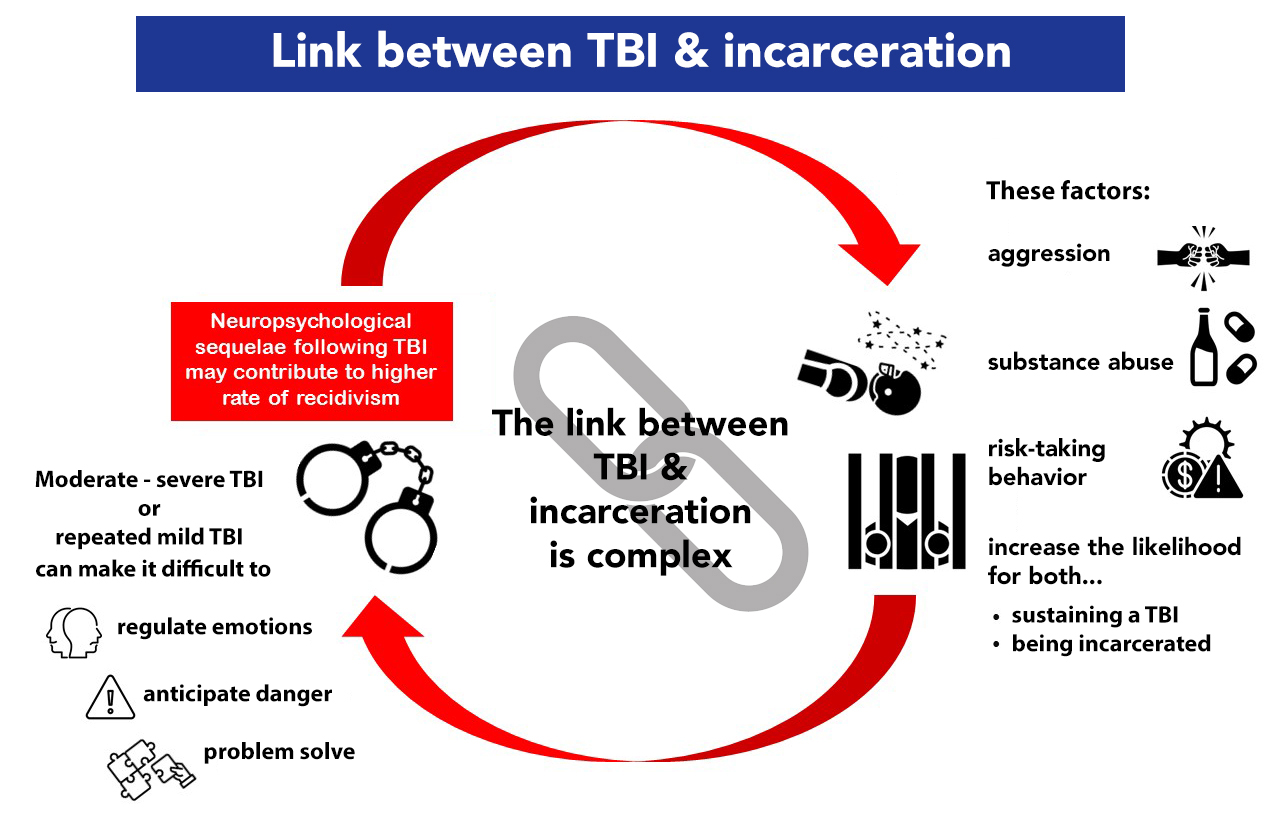
Research suggests that almost half of justice-involved individuals (i.e. individuals in correctional or detention facilities) have sustained at least one prior TBI in their lifetime, 38 with prevalence rates ranging from between 12 and 82% for youths and 23-87% for adults. 39, 40, 41 Although justice involvement can span a number of permutations (e.g., court hearing, probation/parole), the impact of TBI is especially pronounced during incarceration. The link between TBI and incarceration is complex and influenced by several factors. For example, factors contributing to risk for sustaining a TBI also increase the likelihood of engaging in behaviors that may lead to incarceration (e.g., aggression, using substances, general risk-taking behavior). Furthermore, the neuropsychological sequelae following TBI may also contribute to a higher risk of recidivism. For example, sustaining a TBI, particularly a moderate to severe TBI, or repeated mild brain injuries can make it more difficult to regulate emotions, anticipate dangerous situations, and problem-solve. This in turn may increase the likelihood of offending behavior. The extent to which TBI shifts a person's trajectory towards incarceration is influenced by pre-existing factors, the nature of the injury, and circumstances post-injury.
TBI & Justice-Involved: Background
In addition to increased incarceration risk, individuals with a history of TBI may experience unique challenges while incarcerated when compared to those who have not sustained a TBI. They may be more likely to use substances or have a psychiatric disorder, thereby exacerbating the common emotional challenges associated with justice-involvement. 42 Furthermore, an array of other types of TBI-related challenges are also likely to negatively impact the individual's experience while incarcerated. Examples include:
- language & communication (e.g., difficulty understanding and following legal proceedings)
- attention, memory & processing speed (e.g., following directions, slowed responses to directives)
- anger, irritability, and impulse control (e.g., increased conflict with other inmates)
- initiation, planning and problem-solving (e.g., difficulty initiating requests for assistance)
- judgment and decision-making (e.g., detecting and avoiding dangerous situations)
These deficits and challenges often result in higher rates of infractions and disciplinary action.
Please visit our Interventions page for recommendations and treatment strategies.TBI & Homelessness: Introduction
Rates of traumatic brain injury (TBI) are substantially elevated among those with a history of homelessness relative to the general population. 43 For example, one review noted the approximate lifetime prevalence of mild TBI among homeless individuals was 53.1% and 22.5% of homeless individuals had a lifetime moderate or severe TBI. 44
TBI & Homelessness: Background
Unfortunately, TBI and housing instability can, at times, signal a vicious cycle. For example, those who have experienced a TBI, especially chronic, repeated injury or those of moderate to severe severity, can experience neurocognitive deficits, including impact to memory or attentional functioning. 39, 45, 46, 47 Such deficits can impact these individuals' ability to navigate occupational and financial obligations. 48, 49 This, in turn, can result in housing instability and, at times, homelessness.
Conversely, those experiencing homelessness are at elevated risk for exposure to violence (e.g., physical assault) which can result in TBI. 50 Moreover, individuals with a history of homelessness have notably high rates of chronic health conditions (e.g., hypertension) and mental health sequelae (e.g., depression, serious mental illness, substance use) which can further exacerbate neurocognitive and psychosocial functioning. 51, 52, 53, 54, 55, 56
Please visit our Interventions page for recommendations and treatment strategies.TBI & Youth: Introduction
In the United States, studies report incidence rates of pediatric TBI ranging from 70-75 per 100,000. 57 While most injuries are classified as mild, there are approximately 50,000-60,000 children hospitalized for TBI each year. Children and adolescents are most at risk for TBI during the ages of 0-2 years old and 15-18 years old. 57
TBI & Youth: Background
There are many similarities in the diagnosis and conceptualization of TBI in youth and adults. As with adults, TBI severity among children is classified as mild, moderate, or severe. However, Abusive Head Trauma (AHT), which includes shaken baby syndrome, is a form of TBI unique to the pediatric population. The cause of AHT is physical child abuse and is most common in children under the age of 5. This type of injury is preventable. Often symptoms associated with AHT are serious and long-lasting. For more information regarding AHT see: CDC — Preventing Abusive Head Trauma in Children.
Please visit our Interventions page for recommendations and treatment strategies.