Rocky Mountain MIRECC TBI Toolkit
Justice Involved Pages: Home | TBI & Incarceration | TBI-Related Problems |
Screening/Assessment | Management & Intervention | Resources
SCREENING AND ASSESSMENT
Jump to: Screen for TBI History | Assess for TBI & Co-Occurring | Practical Application
Commission on Safety and Abuse
The Commission on Safety and Abuse in America’s Prisons (2006) and experts in TBI recommend appropriate screenings, evaluations and treatment for inmates. This includes:
- Routine screening for history of TBI
- Screenings related to substance use and other comorbidities,
- Further evaluations for those indicated (to assess for behavioral concerns, psychological sequelae and cognitive concerns)
- Education for personnel about how to manage and support individuals with TBI
Advice to the Counselor: Screening and Assessment
- Explain to offenders what the screening and assessments are, how the information will be used, and that you will share feedback about the results of the screening and assessments once completed. Advise the offender that the information may help officers and therapists engage them in supervision and treatment in a way that will help them be successful.
- It is critical to administer screening and assessment instruments in a way that encourages honesty. Offenders often think the results of these screenings will be used against them and may try to skew the results to influence the outcome of a trial or supervision.
- The consequences of honest or dishonest responses should be clarified with the offender.
- Counselors should use available collateral information, such as drug testing results, to verify the accuracy of the information.
- Consider re-administering screenings and assessments if new information comes to light during the supervision or therapeutic process that would warrant the process being re-engaged.
Screening for TBI History and Co-Occurring Conditions
Screening for TBI history
Screening for TBI is an important first step in identifying a history of TBI in justice-involved individuals. Screening can be completed as part of a general intake or initial evaluation. There are several tools that can be used to screen for TBI history. Most of these tools are brief and can be easily incorporated in existing forms and templates. Some of these tools are being used or have been validated in justice-involved populations.
| TBI Screening Tool | Description | Administration | Validated in Correctional Settings |
|---|---|---|---|
| Ohio State University Traumatic Brain Injury Identification Method (OSU TBI-ID) | First 5 items of the OSU TBI-ID asking for recall of blows to the head or neck in high velocity of forces. | 5 minutes. No fee for use. Health care and social service providers can be easily trained on this measure via web-based modules at https://tbi.osu.edu/modules Also download Ohio State University TBI Identification Method — Interview Form | Yes |
| Brain Injury Screening Questionnaire (BISQ) | Structured questionnaire that characterizes incidence and severity of lifetime exposure of TBI, as well as symptoms in attention/memory, depression, anxiety/mood, aggression/impulsivity, depression, and physical symptoms. | May be administered via interview or self-administration and can be conducted as self- or proxy-report assessment. There are costs associated obtaining the BISQ which includes access to it and training, as well as a system for scoring and clinical report. More information | Yes |
| Traumatic Brain Injury Questionnaire (TBIQ) | Structured interview regarding frequency and severity of instances of head injury, including cognitive and behavioral symptoms. | 15 minutes. No fee for use. | Yes |
| Brain Check Survey (BCS) | A parent-completed screening tool used to establish a credible history of brain injury, which, in turn, triggers a thorough evaluation of difficulties encountered by students in the classroom | 15-20 minutes. More information |
Unknown |
Need Something Even Briefer?
At the very least, asking a single yes or no question asking the youth or adult offender whether he or she has experienced a blow to the head (such as by a fall, fight, or accident).
Screening for Substance and Mental Health Problems
Screening and in-depth assessment are important first steps in treating substance and mental health disorders; currently no comprehensive national guidelines for screening and assessment approaches exist in the criminal justice system. In the absence of such guidelines, the Substance Abuse and Mental Health Services Administration (SAMHSA)/Center for Substance Abuse Treatment (CSAT) has compiled some information that can help clinicians and counselors develop effective screening and referral protocols to:
- Screen out offenders who do not need substance abuse or behavioral health treatment
- Assess the extent of offenders' treatment needs to make appropriate referrals
- Ensure that offenders receive the treatment that they need, rather than being released into the community with a high probability of re-offending
Advice to the Counselor: Screening for Co-Occurring Disorders
- Screening and assessment for co-occurring disorders should occur on entry into the criminal justice system, given the high prevalence of co-occurring disorders in this population.
- Individuals in community corrections or jail settings may need to be detoxified before screening for co-occurring disorders. The acute symptoms of alcohol or drug use and the residual effects of detoxification can mimic a wide variety of mental disorders, including anxiety, bipolar disorder, depression, and schizophrenia.
| Screening Measure | Description | Administration | Validated in Correctional Settings |
|---|---|---|---|
| AUDIT-C | A 10-item screening questionnaire to identify persons whose alcohol consumption has become hazardous or harmful to their health. | Total administration and scoring time: 3 minutes No fee for use Download |
Yes |
| CAGE Questionnaire | Brief questionnaire to detect alcoholism. | Total administration and scoring time: 2 minutes No fee for use Download |
No |
| Drug Abuse Screening Test (DAST) | A 28-item instrument to identify individuals who are abusing psychoactive drugs; and the degree of problems related to drug use and misuse. | Total administration and scoring time: 5 minutes Minimal fee for use Download |
Yes |
| Simple Screening Instrument for Substance Abuse (SSI-SA) | A 16-item screening instrument that examines symptoms of both alcohol and drug dependence | Total administration and scoring time: 10 minutes No fee for use Download |
Yes |
| Screening Tool | Description | Administration | Validated in Correctional Settings |
|---|---|---|---|
| Beck Depression Inventory II (BD-III) | 21-item questionnaire used to screen for the presence and rate the severity of depression symptoms. | Total administration and scoring time: 10 minutes Fee for use Available at: www.psychcorp.com |
Yes |
| Patient Health Questionnare-9 (PHQ-9) | 9 item questionnaire used to screen for depression | Total administration and scoring time: 5 minutes No fee for use Available at: http://www.phqscreeners.com/ |
No |
| Generalized Anxiety Disorder 7 item Scale (GAD-7) | 7 item questionnaire used to screen for generalized anxiety | Total administration and scoring time: 5 minutes Minimal fee for use Available at: http://www.phqscreeners.com/ |
No |
| Mental Health Screening Form-III (MHSF-III) | 18 item questionnaire to screen for present or past symptoms of most of the major mental disorders; yes/no responses | Total administration and scoring time: 10-15 minutes No fee for use Available at: |
Yes |
| Trauma History Questionnaire (THQ) | 24-item measure that examines experiences with potentially traumatic events using a yes/no format. | Total administration and scoring time: 5-10 minutes No fee for use Available at: https://ctc.georgetown.edu/toolkit |
Yes |
| PTSD Checklist-for DSM V | 20-item self-report measure that assesses the DSM-5 symptoms of PTSD | Total administration and scoring time: 5-10 minutes No fee for use Available at: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp |
No (PCL-C for DSM-IV has been used in correctional settings) |
For additional information regarding screening and assessment of co-occurring disorders in the justice system, see http://www.pacenterofexcellence.pitt.edu/documents/ScreeningAndAssessment.pdf
Assessing for TBI, Co-Occurring Conditions and Neurocognitive Functioning
Assessing for TBI History
While screening tools may assist in the identification of history of TBI, assessment measures are designed to determine whether specific diagnoses and/or deficits are present. The purpose of an assessment is to gather detailed information needed to develop a treatment plan that meets the individual needs of the person. Depending on the goals/outcomes needed and the level of complexity involved, a full evaluation may be indicated. Once possible/probable TBI history has been identified, providers in the juvenile justice system can adopt evidence-based assessment tools that provide systematic methodology to capture important details about a person’s history of injury to inform diagnosis and treatment/management strategies.
Generally, an in-depth assessment will need to be completed by psychologist/neuropsychologist. When indicated, one such assessments with well-documented validity and reliability is the Ohio State University TBI Identification (OSU-TBI-ID) Method - a structured interview that probes for specific details of injury history over the lifetime and allows the practitioner to determine level of severity and subsequent diagnostic impressions. It also provides questions to assess for history of multiple mild injuries, which may be prevalent in this particular population. Learn about the Ohio State University TBI Identification Method.
After information regarding TBI history has been gathered and a history of probable injury or injuries has been confirmed to establish diagnosis, it can be helpful to assess if and how symptoms associated with TBI may be impacting the client's life. Several tools are available to facilitate this process. These tools can be found in the TBI 101 Section of this website.
Assessment of Co-Occurring Conditions
After screening, a full assessment evaluation may be indicated to gather key information to collaboratively conceptualize the problem and to develop a treatment plan. This generally requires a professional trained in psychology/psychiatry. Therefore, criminal justice professionals may utilize in-house clinical providers or refer out to community-based providers when an in-depth assessment is indicated. Mental health and substance use disorders are often assessed in the context of each other and seek to provide the following: presence/absence of co-occurring disorder; client’s readiness for change; and strengths and deficits that may affect treatment planning. The following assessments have been found to be valid and reliable tools in assessing for comorbid substance use or mental health disorders in individuals with histories of TBI.
| Screening Tool | Description | Administration |
|---|---|---|
| Diagnostic Assessment Comprehensive Addiction and Psychological Evaluation (CAAPE) |
CAAPE is a comprehensive tool that can be used for diagnostic purposes as part of a routine clinical intake when both substance use disorders and mental health disorders need to be considered. CAAPE is a copyrighted instrument. For purchase information, visit Evince Clinical Assessments |
It takes approximately 35-50 minutes to complete the evaluation. |
| Symptom Severity Assessment The Brief Addiction Monitor (BAM) |
It includes both symptom level outcomes as well as functional outcomes. Download the BAM here |
The BAM is a 17-item assessment that can be administered by a clinician or completed as a self-administered questionnaire for clients involved in outpatient substance abuse programs. |
| Screening Tool | Description | Administration |
|---|---|---|
| Diagnostic Assessment Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (SCID) – Depression Module |
The SCID is a semi-structured interview for making Diagnostic and Statistical Manual of Mental Disorders (DSM) Axis 1 diagnoses. It is divided into modules. The mood disorder module can be used to assess mood disorders, including major depressive disorder. The SCID development team has completed a final draft of the SCID for DSM-5 and is currently revising the User’s Guide. For more information, including ordering information. |
|
| Mini-International Neuropsychiatric Interview (MINI) | The MINI is a short structured diagnostic interview for DSM-IV and ICD-10 psychiatric disorders. For more information. |
The entire tool can be administered in approximately 15 minutes, though the depression module can be used alone. |
| Symptom Severity Assessment Beck Depression Inventory-II (BDI-II) |
The Beck Depression Inventory-II (BDI-II) contains 21 items that are specifically designed to assess DSM-IV criteria for symptom severity of depression. Purchase the BDI-II here |
*Note: The BDI-II should be scored using a cut score of 19 for individuals with a mild TBI and 35 for individuals with moderate to severe TBI (Homaifar et al, 2009). Reference: Homaifar, B., Brenner L., Gutierrez, P., Harwood, J., Thompson, C, Filey, C., et al. (2009). Sensitivity and specificity of the Beck depression inventory-II in persons with traumatic brain injury. Arch Phys Med Rehabilitation, 90(4):652–6.10.1016/j.apmr.2008.10.028 |
| Screening Tool | Description | Administration |
|---|---|---|
| Diagnostic Assessment Clinician-Administered PTSD Scale for DSm-5 (CAPS-5) |
The Clinician-Administered PTSD Scale-5 (CAPS-5) is considered to be the ‘gold standard’ for assessing and diagnosing PTSD. The previous CAPS was updated to incorporate the DSM-V PTSD diagnostic criteria. For information about the changes from the previous version of the CAPS For training on the use of CAPS Clinicians may request a copy of CAPS here |
The CAPS-5 is a 30-item structured interview that can be used to make a current or lifetime diagnosis of PTSD as well as to track PTSD symptoms over the past week. |
| Symptom Severity Assessment PTSD Checklist for DSM-5 (PCL-5) |
Download information about the PCL-5, including information about the changes from the previous PCL-5 Master’s level providers may request a copy of the PCL-5 |
Please note that the PCL-M has been updated to reflect the DSM-V criteria. The new measure has not yet been validated with individuals with a history of TBI. |
Neurocognitive Functioning
Neurocognitive screening can be an important aspect of care among justice involved populations. Screening provides an efficient way to allocate limited resources to individuals with greatest need, while also informing accommodations and targeted interventions to mitigate the impact of deficits on functioning. While there are no established methods for neurocognitive screening that have been adapted for routine use in criminal justice settings, below are examples of brief measures that have been used with justice-involved populations.
| Screening Tool | Description | Administration | Validated in Correctional Settings |
|---|---|---|---|
| MoCA—Montreal Cognitive Assessment | Measures the following domains of functioning: attention/concentration, executive functions, memory, language, visuo-constructional skills, conceptual thinking, calculations, orientation | Total administration and scoring time: 20 minutes Fee for use: $0; $125 certification fee to train each proctor (recertification required every two years) Available at: www.Mocatest.org Proctor: individuals who complete an online certification (no degree required). Supervision required by healthcare professionals with expertise in cognitive field such as neuropsychologists, neurologists, occupational therapists and psychiatrists |
Yes, but potential lack of sensitivity to more specific cognitive deficits in populations using alcohol and other drugs |
| Neuropsychological Assessment Battery- Screening Module (NAB) | Domains assessed: Attention, language, spatial, memory, executive function. Has applications for use in individuals with co-occurring disorders. | Total administration and scoring time: 45 minutes Fee for use: $7 per administration. Additional fees include: Start up costs, screening module kit, NAB replacement record forms, replacement response booklets, and replacement summary/profile forms Proctor: LPC or LAC or CACIII with masters degree in related field (OR supervised by one of the above). Available at: www.parinc.com/products/pkey/260 |
Yes |
| Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) | Domains assessed include: Immediate memory, visuospatial/constructional language, attention, delayed memory | Total administration and scoring time: 30 minutes Minimal fee for use per administration; Additional fees for Combo Kit (stimulus books, coding templates and manual), and replacement record forms. Available at: http://www.Pearsonclinical.com Proctor: Individual trained to administer test (no degree required). Supervision by: doctorate in psychology, education or related field, OR LPC with additional training |
Yes |
| The Automated Neuropsychological Assessment Metrics (ANAM) | 18 item questionnaire to screen for present or past symptoms of most of the major mental disorders; yes/no responses | Total administration and scoring time: 20-25 min $15 per administration; $500 for license to use; requires computer and mouse Proctor: Bachelor’s degree in related field; supervision can be completed by non-neuropsychologists with training Order from: www.vistalifesciences.com |
Lack of information regarding how sensitive and specific screen is with incarcerated, probation or justice involved population; Not tested with substance abuse population |
| Mental Mini Status Exam (MMSE) | Domains assessed: orientation, memory, attention, naming, verbal/written commands, spontaneous sentence writing, copying of complex polygon | Total administration and scoring time: 5-10 minutes No fee for use Proctor and supervision by: bachelor’s degree in a related field plus satisfactory completion of related coursework OR a license or certification from an agency that requires appropriate training and experience in the ethical and competent use of psychological tests. Order here |
Yes |
Practical Application
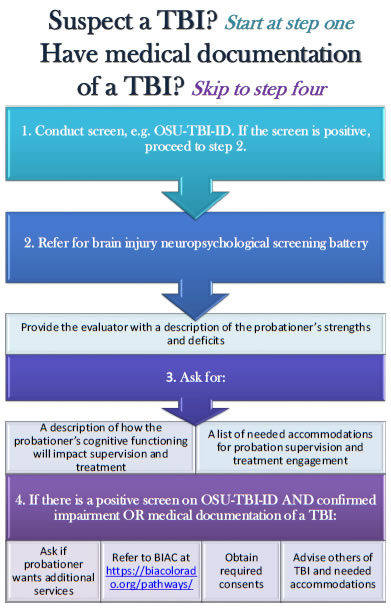
The following infographic demonstrates a practical application. This infographic can be downloaded for easy reading.
| IMPAIRMENT | SIGNS | ACCOMMODATIONS |
|---|---|---|
| Attention | Fidgets, squirms in seat, can’t sit still; Interrupts conversation; Low frustration tolerance; Talks excessively; Off topic; Inability to inhibit impulses | Work on only one task at a time; Have client participate in discussion development of case plan; Reduce distractions; Meet in quiet environment; Use verbal (e.g. “look”, “listen”) non-verbal (e.g. eye contact) cues |
| Inhibition | Fidgets, squirms in seat, can’t sit still; Interrupts conversation; Talks excessively; Not able to respond to multi-step instructions; Acts on the first thing that pops into their mind; Unable to verbally, physically, or mentally “put on the brakes”; Difficulties with transitions (area to area, task to task) | Provide help create structure routine; Mindfulness; Provide cuing; Direct, honest, kind feedback; Prepare for transitions |
| Processing Speed | Slow to respond to questions; Appears to not be paying attention; Looks confused; Doesn’t follow instructions | Provide additional time to review information; Speak slowly, making sure the client understands (ask them to rephrase back to you what they heard); Offer assistance with completing forms; Utilize checklists a written schedule of routines; Provide written cues to organize information (e.g. “first do this, then do this”) |
| Memory Loss | Can’t remember more than one thing at a time; Can’t remember details; Appears disorganized; Appears to have an “attitude” problem; Appears manipulative | Repeat information summarize; Teach client to use a reminder system, e.g. planner; Teach “chunking” as a way to aid in retention; Stick to routine as much as possible; Keep information tangible relevant |
| Sensory Motor | Appear overwhelmed; Emotional melt downs; Irritable, short fused; May appear oppositional; Shuts down; Complains of physical ailments | Keep environment quiet; Keep noise lights to a minimum; Keep sessions short to minimize the onset of headaches fatigue; Schedule rest periods breaks from planned activities |
| Language / Social Pragmatics | Do not interpret body language; Use inappropriate eye contact; May get in your space; May say either too little or too much; Have little insight or awareness of how their behavior may be inappropriate | Provide direct, structured, concrete feedback; Do not rely on body language to convey a message; Role play; Provide shaping, cueing, fading; Videotaping interactions |
| Receptive Language | Confused; May say “huh” frequently; Followers; Struggle with abstract language/sarcasm; May withdraw | Be direct; Avoid abstract humor, sarcasm, metaphors, colloquialisms; Allow wait time for person to process what has been said; Provide instructions/directions slows one at a time; Ask if it would be helpful to repeat or rephrase your message; Let the individual know that you value their input, thoughts feelings |
| Expressive Language | Poor grammar or immature speech; Difficult to follow in conversation; Difficulty staying on topic; Difficulties navigating social rules; May withdraw | Redirect if the client is off topic; Provide opportunities to practice expression; Role play common real life conversations; Teach individual to rehearse silently before replying; Be patient allow the client time to respond |
| Visual / Spatial | Appear clumsy; overwhelmed; Inability to write clearly; Reading difficulties; Does not understand information from charts or graphs; Gets confused when reading a map; Inability to read social cues or facial expressions | Provide precise and clear verbal directions; Simplify visual information given; Check for understanding; Ask if it would be helpful to repeat or rephrase your message; Enlarge written materials; Provide support in organizing writing/expressing thoughts; Reduce clutter in work area |
| Initiation | Appears lazy or spacey; Appears unmotivated; Follower; Needs constant cueing; Lags in independent living skills | Provide written instructions; Ask client to repeat instructions to ensure comprehension; Use underlining or highlighting for significant instructions; Break complex directions into simple steps assign action items; Utilize color coding; Help the client get started; Repeat instructions or interventions multiple times in multiple ways |
| Planning | Rigid thinking; Can’t think of more than one way to do something; Gets confused; Often late and unprepared; Difficulties doing more than one task at a time; Difficulties organizing thoughts | If client appears stuck, ask, “What should you do first?” or “What happens next?”; Break each expectation down into clear steps; Teach time management and prioritizing; Teach how to develop short term and long term goals; Connect new information with what they already know; Develop and practice schedules and routines; Provide a written schedule |
| Mental Flexibility | Perseverate; Difficulties taking feedback; Resistant; Can appear stubborn or argumentative; May appear to lack empathy | Develop practice routines; Plan ahead for changes; Prepare for transitions; Help develop alternative plans; Ensure goals are broken down into smaller, achievable tasks; Provide respectful feedback to potential or obvious problem areas |
| Organization | Inability to create or maintain orderliness in thoughts, activities, materials and the physical environment; Resistant; Confused; Unable to do more than one step in a task; Conversations may be disjointed; Difficulties answering open ended questions; Appears to have memory issues and loses things easily | Provide step by step instruction and present information in small, concise, concrete steps; Use checklists for tasks; Suggest and model the use of notebooks for communication and information gathering |
| Reasoning | Concrete thinkers; Can’t think of alternative solutions; Difficulties answering open ended questions; Difficulties learning from experience, cause effect | Point out possible short long-term consequences of decisions; Teach step-by-step approaches to problem solving; Avoid open-ended questions; Speak concretely; Be clear on expectations consequences of risk taking behaviors; Be supportive continually identify strengths |
| Emotional / Behavioral | Over/under reaction; Difficulties with anger management;Meltdowns; Can appear emotionally “flat”; Difficulties making friends; Can appear argumentative | Minimize anxiety with reassurance, education structure; Avoid focusing only on deficits; Don’t misinterpret lack of emotion as a lack of interest; Suggest breaks if the client becomes irritable or agitated; Use mindfulness exercises to aid clients in identifying emotional states; Role play |
Site Map
Contact Information
Denver
Rocky Mountain Regional VAMC (RMR VAMC)
1700 N Wheeling St, G-3-116M
Aurora, CO 80045
720-723-6493
Salt Lake City
VA Salt Lake City Health Care System
500 Foothill DR
Salt Lake City, UT 84148
801-582-1565 x2821




















